A new mRNA cancer vaccine creates lasting immunity in patients, with some remaining cancer-free for years
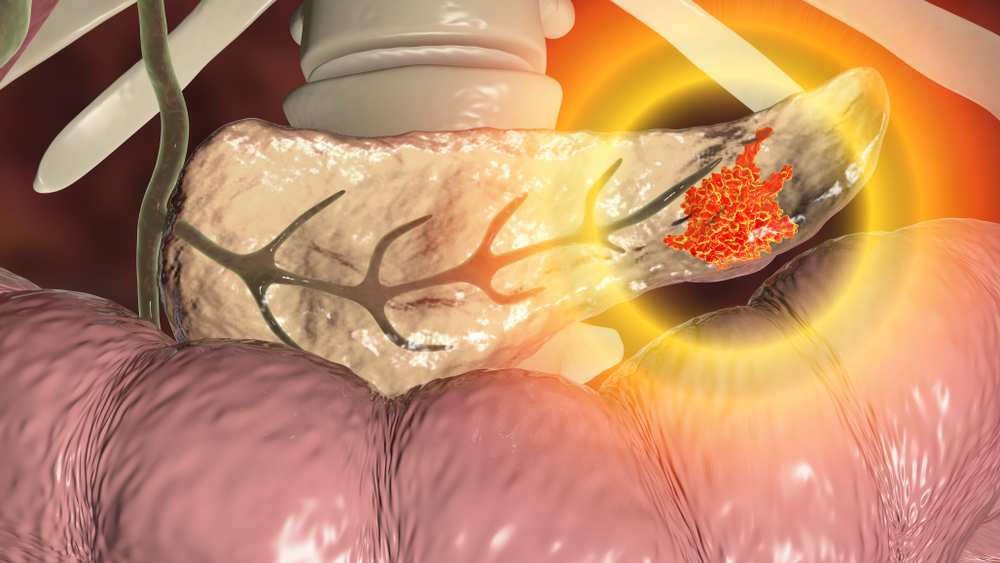
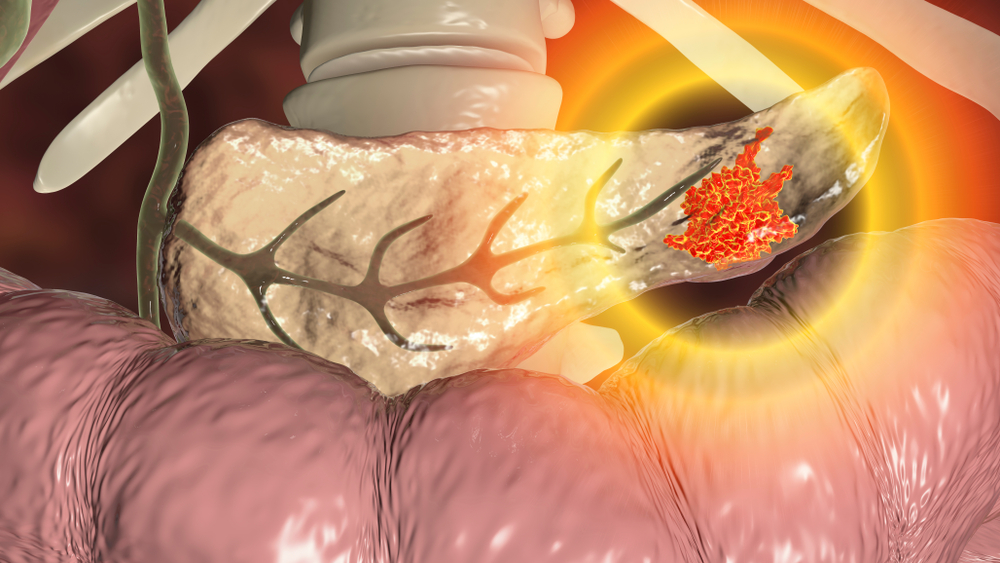
For decades, a diagnosis of pancreatic cancer has carried a grim prognosis. Often detected late and resistant to most treatments, the disease is among the deadliest cancers, with only about 13% of patients surviving five years after diagnosis. Families and patients alike know too well the sense of urgency for new options—therapies that not only extend life but offer a chance at lasting remission.
Now, a promising experimental approach is challenging the long-standing narrative of inevitability. Scientists at Memorial Sloan Kettering Cancer Center, in collaboration with BioNTech and Genentech, are testing a personalized mRNA cancer vaccine that has shown the ability to train the immune system to recognize pancreatic tumors as foreign and fight them off. In early clinical results, some patients have remained cancer-free for years, with immune responses persisting long after treatment.

A Breakthrough in Pancreatic Cancer Treatment
For decades, pancreatic cancer has been one of the most formidable diagnoses a patient can receive. Despite advances in surgery, chemotherapy, and targeted therapies, survival rates remain dishearteningly low—only about 13% of patients are alive five years after diagnosis, according to the American Cancer Society. Against this backdrop, researchers at Memorial Sloan Kettering Cancer Center (MSK) are exploring an innovative path: a personalized mRNA-based cancer vaccine called autogene cevumeran.
Unlike preventive vaccines that protect against viruses, this therapeutic vaccine is designed to treat cancer by training the immune system to recognize and attack tumor-specific proteins known as neoantigens. These neoantigens arise from genetic mutations within cancer cells, making them distinct from healthy cells. By delivering instructions through messenger RNA (mRNA), the vaccine teaches the immune system to spot these abnormal proteins and mobilize T cells—the body’s natural cancer fighters—against them.
Early results from a phase 1 trial of 16 patients with pancreatic cancer are offering cautious but genuine hope. Half of the participants mounted a strong immune response after receiving the vaccine, and among those responders, the majority remained cancer-free at a three-year follow-up. Even more striking, in some individuals, vaccine-activated T cells were still detectable and functional nearly four years after treatment. “These results suggest this investigational therapeutic mRNA vaccine can mobilize anti-tumor T cells that may recognize pancreatic cancers as foreign, potentially years after vaccination,” said Dr. Vinod Balachandran, the trial’s principal investigator and director of MSK’s Olayan Center for Cancer Vaccines.
These findings, though preliminary, mark a critical step in reimagining how cancer can be treated—shifting from approaches that broadly suppress tumor growth to ones that enlist the body’s own immune system in a sustained fight against recurrence

The Science Behind a Personalized Vaccine
At the heart of this new therapy is a deceptively simple idea: teach the immune system to see cancer as a threat. Yet the execution requires extraordinary precision. After a patient’s tumor is surgically removed, scientists analyze its genetic makeup to identify mutations most likely to produce recognizable neoantigens. Out of hundreds of possible genetic alterations, only a select group of around 20 are chosen to form the blueprint for the vaccine. Using messenger RNA (mRNA) technology—the same platform that enabled rapid development of COVID-19 vaccines—researchers encode instructions for the body to produce these tumor-specific proteins.
This vaccine is not a “one-size-fits-all” product. Each batch must be tailored to the patient, reflecting the unique molecular fingerprint of their cancer. Once administered, the mRNA enters immune cells, prompting them to generate the neoantigen proteins. These proteins act like warning flags, signaling to T cells that cancer cells carrying the same mutations are intruders. What makes this approach so compelling is its potential durability: rather than offering a fleeting response, the immune system retains a “memory” of these neoantigens, equipping it to mount future defenses against recurrence.
Developing such a vaccine presents logistical and scientific hurdles. Unlike preventive vaccines that can be mass-produced, therapeutic cancer vaccines must be manufactured individually, often across international borders. In this case, tumor samples are shipped to BioNTech’s facilities in Germany, where the vaccine is designed and produced before being returned for patient treatment. Despite this complexity, the collaboration between MSK, Genentech, and BioNTech has demonstrated that it is not only possible, but scalable enough to move into larger trials. The scientific advances in genomic sequencing, computational biology, and biotechnology over the last decade have been crucial in making what once seemed aspirational into a tangible therapy now tested in patients.

Clinical Trial Results and What They Mean
The first trial of autogene cevumeran enrolled 16 patients with pancreatic cancer who had undergone surgery to remove their tumors. They received the vaccine in combination with chemotherapy and an immunotherapy drug. At the 1.5-year follow-up, researchers observed that half of the patients developed a measurable T cell response, and those who responded had a delayed recurrence of cancer compared with those who did not. Now, with results extending out to a three-year median follow-up, the picture is becoming clearer: six out of the eight responders remain cancer-free, while the two who relapsed had weaker immune activity.
Perhaps most significant was the persistence of vaccine-induced T cells. These cells, undetectable before vaccination, remained active in patients’ blood for more than two years, with some still identifiable nearly four years after treatment. This endurance is rare in cancer therapies, where immune responses often fade over time or are suppressed by the tumor itself. Importantly, chemotherapy did not appear to blunt the vaccine’s effectiveness, suggesting the approach could integrate with existing treatment regimens without being undermined by them.
While these findings are undeniably promising, researchers are careful to temper optimism with caution. The trial was small and lacked a control group, meaning it is not yet possible to definitively prove the vaccine was responsible for the improved outcomes. That is why a phase 2 trial involving around 260 patients worldwide is now underway. This larger, randomized study will compare outcomes between patients receiving the vaccine alongside standard therapies and those receiving only standard treatment. If results hold, the trial could mark a turning point not just for pancreatic cancer, but for the broader field of cancer immunotherapy.

The Challenge of Pancreatic Cancer
To fully appreciate the significance of these findings, one must understand the formidable nature of pancreatic cancer. Often referred to as a “silent killer,” the disease is difficult to detect early because symptoms usually appear only after it has advanced. Even when surgery is possible, recurrence rates are high, and the cancer often resists conventional treatments such as chemotherapy and radiation. That is why survival rates have remained stubbornly low compared with other cancers.
Researchers have long sought to harness the immune system against pancreatic cancer, but the tumor’s biology has posed obstacles. Its dense tissue structure and complex microenvironment create a barrier that shields it from immune attack. Moreover, most pancreatic tumors manage to evade recognition by the immune system altogether, cloaking themselves in a way that prevents T cells from detecting them as abnormal. For decades, this ability to “hide in plain sight” has made immunotherapies that succeed in other cancers largely ineffective against pancreatic cancer.
The work of Dr. Vinod Balachandran’s team helped illuminate why some rare patients manage to beat the odds. They discovered that long-term survivors often carry tumors with neoantigens that the immune system can detect, triggering lasting T cell responses. In some of these exceptional patients, T cells recognizing tumor neoantigens remained in circulation for more than a decade after surgery. These insights were pivotal in inspiring the development of a vaccine capable of recreating that natural immune protection in others who would otherwise face a bleak prognosis.
A Collaborative Effort in Innovation
The path to this breakthrough has been as much about collaboration as it has been about science. The idea of using mRNA technology for cancer treatment was gaining traction just as the COVID-19 pandemic accelerated global investment and innovation in vaccine platforms. It was around this time that BioNTech, already exploring individualized mRNA immunotherapies, connected with MSK researchers to adapt the technology for pancreatic cancer. Genentech, with its expertise in large-scale clinical development, soon joined the effort.
This multinational collaboration has enabled the vaccine to move from theory to early clinical reality in just a few years. Equally important, it reflects a shift in how cancer research is pursued: combining expertise from basic science, biotechnology, and clinical care. At MSK, the establishment of The Olayan Center for Cancer Vaccines provides a hub for testing and refining next-generation vaccine concepts, not only for pancreatic cancer but also for other aggressive cancers where treatments remain limited.
The effort has also been supported by diverse funding sources, ranging from foundations to federal agencies, highlighting the broad recognition of its potential. The project’s progress underscores the value of sustained investment in translational research—work that bridges laboratory discovery with patient benefit. Without such support and cooperation, moving a personalized therapy of this complexity from bench to bedside would not be possible.
Looking Ahead: Hope and Responsibility
For patients and families facing pancreatic cancer, the early results of the mRNA vaccine trial offer a rare glimmer of hope. The possibility that a vaccine could provide lasting protection against recurrence, mobilizing the body’s own immune system years after treatment, is extraordinary in a disease long considered nearly untreatable. Yet hope must be matched with patience: larger trials are essential to confirm whether the vaccine can deliver consistent benefits across broader populations.
If successful, the implications reach far beyond pancreatic cancer. The concept of designing individualized vaccines to target tumor-specific mutations could potentially be applied to other cancers that resist existing therapies. This could mark a paradigm shift in oncology, moving toward treatments that are not only more effective but also more personalized, tailored to the unique genetic makeup of each patient’s tumor.
Still, with innovation comes responsibility. Scientists and clinicians emphasize that these therapies must be rigorously tested, ethically deployed, and made accessible to patients who need them most. The promise of personalized medicine cannot be realized if it remains out of reach for all but a few. For now, what matters most is that research continues, patients enroll in trials, and the momentum built by this early success is sustained. For those touched by pancreatic cancer, the message is clear: while challenges remain, the horizon is no longer devoid of possibility.
Loading...

