Pioneering Eye Implant Brings Central Vision Back to Patients With Advanced AMD
For many people living with dry age related macular degeneration, losing central vision is not just a medical challenge but an emotional one that reshapes identity, independence, and daily life. The condition often leaves individuals unable to read, see faces clearly, or engage with the world in the way they once did, and the sense of permanence that comes with this loss can be heavy. Yet a remarkable development is beginning to change that expectation, offering something that no treatment for advanced dry AMD has been able to promise before. A new retinal implant has shown that the restoration of meaningful central vision may no longer be an unreachable possibility.
Across Europe and at Moorfields Eye Hospital in London, a clinical trial testing the PRIMA System has delivered results that have surprised even those who have spent decades studying retinal diseases. With a tiny implant paired with smart glasses and advanced processing technology, patients who previously had no central vision have now been able to read letters, numbers, and even full words. For many, it has reopened the door to once familiar worlds such as books, puzzles, and printed details that had faded into memory. Among them is Sheila Irvine, whose journey through the trial reveals how profound the return of something as simple as a single letter can be.

Image Credit: Shutterstock
A Transformational Step Forward for Central Vision Loss
The PRIMA System is emerging as one of the most significant developments in the effort to address geographic atrophy, the advanced form of dry AMD. Five patients at Moorfields received the implant as part of a wider group of thirty eight participants across five European countries. All participants had lived without central vision before the trial, yet the majority experienced breakthroughs that exceeded expectations. According to the trial results, 84.4 percent of participants regained the ability to read letters, numbers, and words, marking a substantial step forward in a field where available treatments have long been limited.
Patients were able to read up to five lines on an eye chart using the treated eye. This was possible even though none of them had previously been able to read with that eye. These outcomes show not just technical progress but a shift in how researchers understand the potential of artificial vision. Dr Mahi Muqit, a senior vitreoretinal consultant at Moorfields and UCL’s Institute of Ophthalmology, described this advancement as “a new era” in the history of artificial vision. He emphasised that blind patients are finally experiencing meaningful central vision restoration, something no earlier approach had achieved.
The significance extends beyond clinical measurements. Regaining the ability to read supports emotional wellbeing, boosts confidence, and improves day to day independence. Dr Muqit noted that the PRIMA chip operation can be performed by any trained vitreoretinal surgeon in under two hours, which is vital for ensuring that access to this technology can eventually be widened. For many people affected by dry AMD, whose options have remained limited for years, this development brings renewed optimism.

Image Credit: Shutterstock
Sheila’s Experience Returning to the World of Reading
Among the personal stories in the trial, Sheila Irvine’s stands out for its combination of honesty, determination, and hope. Before receiving the implant, she described her vision as “like having two black discs in my eyes, with the outside distorted”. She had lived an active life despite her sight loss, but what she missed most deeply was reading. As she put it, “I was an avid bookworm, and I wanted that back”. The trial offered a chance not only to help herself but also to contribute to research that might support others living with AMD.
Sheila admitted feeling “nervous, excited, all those things” before the procedure. She recalled that “there was no pain during the operation, but you’re still aware of what’s happening”. What mattered most to her was the possibility, however small, of connecting again with the written world that had shaped so much of her life. That possibility became real when she began to see her first letter through the implant, a moment she described as “dead exciting”.
Learning to read again has not been simple for Sheila, but it has been rewarding. She explained that “it’s not simple, learning to read again, but the more hours I put in, the more I pick up”. She now challenges herself daily by looking at prescription labels, studying the small print on tins, and completing crossword puzzles. These tasks encourage her to stretch her abilities and enjoy the improvements she gains over time. The implant has made a meaningful difference to her life and renewed her optimism. As she expressed, “reading takes you into another world, I’m definitely more optimistic now”.
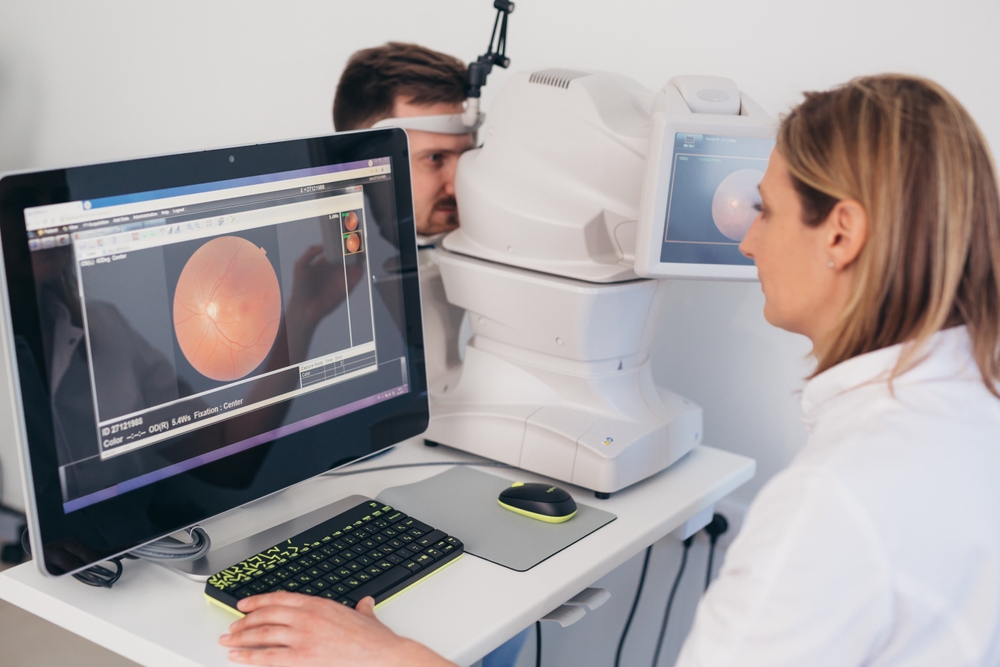
Image Credit: Shutterstock
How the PRIMA System Works Without Replicating Natural Vision
The technology behind the PRIMA System brings together micro engineering, neural stimulation, and advanced image processing. The system has three main components. The first is a wireless retinal implant that measures only two millimetres by two millimetres and is inserted beneath the retina. The second component is a pair of augmented reality glasses equipped with a small camera and a digital projector. The third is a pocket processor that interprets visual information and guides how it is transmitted to the implant.
One month after implantation, once the eye has had time to settle, the chip is activated. The glasses capture the visual scene and send it to the processor, where artificial intelligence algorithms analyse the image and identify the object most important for the user to focus on. The glasses then project this simplified information through the eye as an infrared beam. The chip converts the beam into electrical signals that travel through the retinal cells and optic nerve to the brain, where they are interpreted as visual input.
Although the resulting vision does not replicate natural sight, it creates a form of functional central vision that allows users to read, navigate, and recognise key objects. For people who had no central vision at all before surgery, this represents a significant improvement. Dr Muqit has stressed that restoring the ability to read is a major milestone that improves quality of life and helps restore confidence. The fact that the surgery can be completed efficiently by trained surgeons adds to the practicality of future widespread adoption.

Image Credit: Shutterstock
Growing Optimism in the Field of Artificial Vision
Researchers and advocates within the macular disease community have responded with enthusiasm to the early trial results. Dr Peter Bloomfield, director of research at the Macular Society, described the findings as “encouraging results which indicate an improved quality of life to patients living with dry AMD, particularly GA. Where there is currently no treatment option, this is fantastic news”. He highlighted the promise shown in connecting digital and biological systems, calling it an area with “great potential”.
The PRIMA System builds on earlier work by Pixium Vision, the organisation that originally developed the implant. In 2022, an eighty eight year old woman in the United Kingdom became the first patient in the country to receive the device as part of an earlier stage of research. The technology is now being developed further by Science Corporation in California, suggesting that there is long term interest in refining and expanding its capabilities.
One of the major questions now centres on whether the device will eventually be approved for use in the United Kingdom and whether it could become available through the NHS. The Macular Society is monitoring these developments closely. While approval has not yet been granted, the organisation continues to fund research and offer support to individuals living with macular disease as progress unfolds. The potential benefits extend well beyond reading, touching mobility, independence, and overall wellbeing.

Image Credit: Shutterstock
Rethinking the Future of Vision Restoration
The PRIMA System reflects a shift toward new ways of addressing blindness caused by retinal degeneration. If the technology continues to advance, it could support greater independence for thousands of people who have lost central vision to geographic atrophy. It also opens the door to future innovations in neural interfaces and artificial vision systems that may eventually improve clarity, contrast, and recognition capabilities even further.

Image Credit: Shutterstock
The ripple effects of this work reach beyond ophthalmology. The combination of biological structures with digital processing represents a growing frontier in medicine. As these tools become more refined, they may influence treatments for other degenerative conditions and support a wider range of people who experience sensory loss. The importance of scalable procedures and wider clinical training highlights how essential it will be to ensure equitable access if the PRIMA System becomes approved.
For now, the most meaningful impact lies in individual stories like Sheila’s, where the return of a single letter opens the door to a familiar world that had once slipped away. Her experience invites reflection on how medical innovation can restore not only function but also confidence, curiosity, and connection. It signals a future where blindness caused by dry AMD may no longer define the limits of possibility.
Featurd Image via Shutterstock
Loading...

