Your Brain Could Soon Rebuild Itself After a Stroke Thanks to Dancing Molecules
Every 40 seconds, someone in America suffers a stroke. Doctors rush to restore blood flow, racing against time to save brain tissue and prevent death. But here lies a cruel paradox that has plagued medicine for decades. Saving a life often means watching helplessly as a second wave of damage unfolds.
For years, scientists have researched for a way to stop what happens next. And now, a team at Northwestern University may have found it.
When Saving a Life Creates New Damage
Picture a dam holding back water. A blockage forms, cutting off everything downstream. When workers finally remove that blockage, water rushes through with tremendous force. Something similar happens in the brain during stroke recovery.
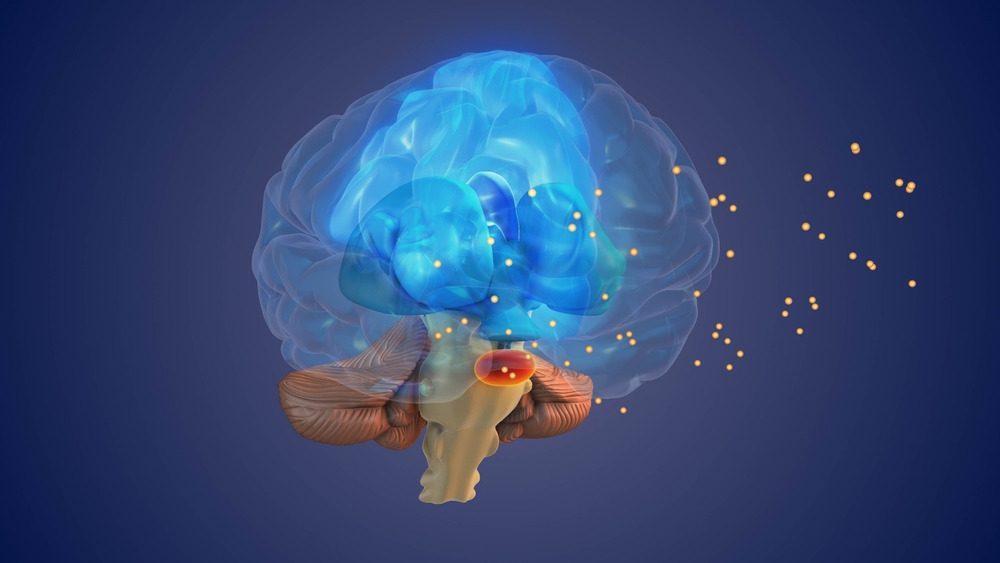
Ischemic stroke occurs when a clot blocks blood flow to the brain. Physicians work quickly to reopen the vessel, either by administering clot-busting drugs or surgically removing the obstruction. Restoring circulation saves lives. But that sudden rush of blood also triggers a cascade of harmful events.
Brain cells begin dying. Inflammation spreads through vulnerable tissue. Harmful molecules that accumulated during the blockage suddenly flood into surrounding areas, causing even more destruction. Disability risk climbs with each passing moment.
Acute ischemic stroke accounts for 80% of all strokes in America and remains one of the leading causes of death and disability worldwide. Severe strokes can leave patients with permanent impairments that affect their ability to work, engage with family, and participate in society. Beyond the personal toll, families and communities bear enormous financial burdens.
Dr. Ayush Batra, associate professor of neurology and pathology at Northwestern University Feinberg School of Medicine, has spent years studying what happens after blood flow returns. He knows the frustration of watching patients survive only to face lasting disability.
“Current clinical approaches are entirely focused on blood flow restoration,” Batra said. “Any treatment that facilitates neuronal recovery and minimizes injury would be very powerful, but that holy grail doesn’t yet exist. This study is promising because it’s leading us down a pathway to develop these technologies and therapeutics for this unmet need.”
Molecules That Dance
Samuel I. Stupp, Board of Trustees Professor at Northwestern, has been working on something unusual. His laboratory created what scientists have nicknamed “dancing molecules” because of how they behave.
Most treatments sit still once injected. Stupp’s molecules move constantly, searching for cellular receptors the way dancers search for partners on a crowded floor. By tuning how these molecules move collectively, researchers can help them find and engage with cells that need repair signals.
In 2021, Stupp’s team published a study showing that a single injection of these dancing molecules could reverse paralysis in mice with severe spinal cord injuries. Nerve fibers grew back. Lost connections reformed. Paralyzed animals walked again.
But that treatment required injecting the therapy directly at the injury site. For spinal cord injuries, doctors can do that. For strokes deep inside the brain, direct injection would require invasive surgery.
Stupp and Batra wondered if they could adapt the technology. Could dancing molecules travel through the bloodstream and find their way into damaged brain tissue on their own?
A Barrier That Blocks Almost Everything
One massive obstacle stood in their way. Between blood vessels and brain tissue sits a protective layer called the blood-brain barrier. It keeps toxins and pathogens out of the brain. Unfortunately, it also keeps most medications out. For decades, promising therapies have failed simply because they could not cross this barrier to reach brain tissue.
Batra calls this one of the most frustrating challenges in neuroscience. Drugs that work beautifully in a lab dish become useless when they cannot reach their target inside a living brain.
But a stroke creates an unexpected opportunity. When physicians restore blood flow to an ischemic brain region, the blood-brain barrier temporarily becomes more permeable. A small window opens, creating a brief opportunity for intervention.
Researchers needed a therapy that could exploit that window. Stupp’s dancing molecules seemed like ideal candidates.
Redesigning the Treatment

For the spinal cord therapy, scientists injected dancing molecules as a liquid that immediately formed a gel-like network of nanofibers. That approach worked well for direct injection but would cause problems in the bloodstream. Gels could form clots, potentially creating new blockages and making the stroke worse.
Stupp’s team dialed down the concentration. At lower doses, the molecules stayed small enough to travel safely through blood vessels. Researchers chose one of their most active formulations, selecting peptide assemblies with highly mobile molecular structures that would have a better chance of slipping through the blood-brain barrier.
Once enough molecules crossed into brain tissue, they could form larger structures to produce a stronger therapeutic effect. Small going in, powerful once inside.
Testing in Real-World Conditions
Many stroke treatments have failed because laboratory conditions do not match what happens in emergency rooms. Batra insisted on a study design that mimicked real clinical scenarios.
Researchers first blocked blood flow in mice to simulate a major ischemic stroke. After 60 minutes, they restored circulation, just as physicians do for human patients. Immediately after reperfusion, mice received a single intravenous dose of the dancing molecule therapy.
Over seven days, scientists monitored the animals for side effects. Advanced imaging techniques confirmed that the therapy traveled to the stroke injury site. Fluorescent labels attached to the molecules revealed them crossing the blood-brain barrier and accumulating in damaged areas.
Mice that received the treatment showed significantly less brain tissue damage compared to untreated animals. Inflammation decreased. Signs of excessive immune response diminished. And researchers observed no toxicity in major organs like the liver, kidneys, or spleen. Samuel Stupp explained what makes the therapy work on multiple fronts.
“You get an accumulation of harmful molecules once the blockage occurs and then suddenly you remove the clot and all those ‘bad actors’ get released into the bloodstream, where they cause additional damage,” Stupp said. “But the dancing molecules carry with them some anti-inflammatory activity to counteract these effects and at the same time help repair neural networks.”
Teaching Nerve Cells to Rebuild
Beyond fighting inflammation, the therapy sends regenerative signals to surviving neurons. It encourages nerve cells to repair themselves, helping nerve fibers called axons grow again and reconnect with neighboring cells.
Scientists call this plasticity, meaning the brain can adapt and rebuild connections after injury. Stupp’s dancing molecules tap into natural repair mechanisms that the brain already possesses but struggles to activate after severe damage.
In earlier spinal cord studies, the therapy formed a network of nanofibers that mimicked the natural structure surrounding nerve cells. By matching this structure and incorporating signals for cellular receptors, the synthetic materials communicated with cells in ways that promoted regrowth.
Brain tissue presents different challenges than the spinal cord, but the underlying principles remain similar. Neurons need signals telling them to survive, grow, and reconnect. Dancing molecules deliver those signals.
Why Crossing the Barrier Changes Everything

For the first time, researchers demonstrated that supramolecular therapeutic peptides can travel through the bloodstream and reach damaged brain tissue without surgery or direct injection. Batra believes this opens possibilities far beyond stroke treatment.
“Add to that a dynamic peptide that is able to cross more readily, and you’re really optimizing the chances that your therapy is going where you want it to go,” Batra said.
Stupp agrees that systemic delivery represents a major advance. Beyond stroke, the technology could eventually help patients with traumatic brain injuries and neurodegenerative diseases like ALS, conditions where effective therapies have long been blocked by the blood-brain barrier.
What Still Needs to Happen

Despite promising results, significant work remains before this treatment reaches human patients. Seven days of observation showed reduced brain damage, but many stroke survivors face cognitive decline that unfolds over months or even a year after their stroke. Researchers need longer studies with more sophisticated behavioral testing to determine whether the therapy supports functional recovery over time.
Batra notes that the treatment seems primed to address secondary injury that occurs long after the initial stroke. Proving that benefit will require patience and careful measurement.
Scientists also want to test whether additional regenerative signals could be incorporated into the therapeutic peptides. Future versions might carry multiple repair signals, producing even better results.
A Complement to Existing Care
No one expects dancing molecules to replace clot-busting drugs or surgical clot removal. Restoring blood flow remains the priority in stroke treatment and will continue saving lives.
But if clinical trials confirm what laboratory studies suggest, this injectable therapy could become a powerful complement to existing approaches. Physicians could administer it immediately after restoring blood flow, protecting the brain during its most vulnerable window, and supporting recovery in the days and weeks that follow.
For the hundreds of thousands of Americans who suffer strokes each year, and for millions more around the world, such a treatment could mean the difference between lasting disability and meaningful recovery.
Right now, doctors can save your life when a clot blocks blood to your brain. Soon, they might also be able to protect what makes that life worth living.
Loading...

