
Imagine trying to stop a wildfire but instead of flames, it’s a slow, creeping silence stealing the voice, the balance, the movement from millions around the world. That’s Parkinson’s disease. It doesn’t shout; it whispers, gradually dimming the spark that once lit up a person’s every gesture and word.
Every year, over 10 million people globally face this invisible thief. And while modern medicine offers tools to ease the symptoms, no treatment has ever stopped it in its tracks until now.
In a twist that feels almost poetic, a cancer drug originally designed to train the immune system to fight tumors is now showing promise as a weapon against Parkinson’s. Scientists have uncovered a critical interaction between two proteins that could be the disease’s main route of attack. And with one precise disruption, they’ve managed to block the destruction before it starts.
So what happens when the science of one battlefield opens a door to hope on another?
Understanding Parkinson’s Disease
Parkinson’s rarely announces its arrival with sirens it tip-toes in, muffling the body’s once-fluent rhythm, one subtle tremor at a time. More than 8.5 million people worldwide live inside this slow-burning storm, according to recent World Health Organization estimates (2022). Yet the numbers tell only half the story. Behind every statistic is someone who can recall the exact moment a button suddenly felt too small, a signature wavered, or a favorite song became harder to dance to.
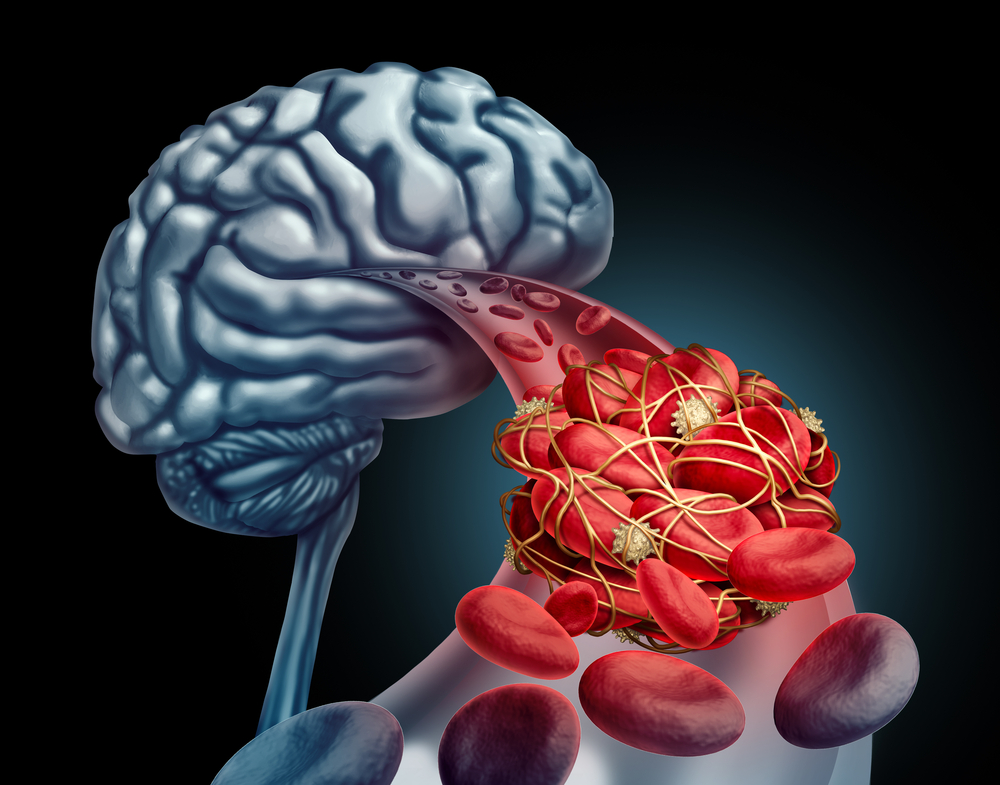
At its core, the disorder is a dopamine drought. Deep within the brain’s substantia nigra, specialized neurons craft this neurotransmitter the chemical spark that turns thought into movement and mood. When misfolded clumps of the protein alpha-synuclein (the notorious “Lewy bodies”) spread through these cells, the factory falters. Production stalls, and everyday actions tying a shoelace, meeting a friend’s gaze, even standing tall begin to feel like feats of strength.
🚨FDA approves Talectrectinib for ROS1 positive locally advanced or metastatic NSCLC.
— Dr. Saadvik Raghuram y (@saadvikdr) June 25, 2025
➡️ Response rates in TKI naive (85-90%)
➡️ ORR in patients with prior TKI (52%)
➡️ CNS response rates in TKI Naive (73%), prior TKI (63%)
➡️ Watch out for Dizziness, QTc@OncoAlert@SuyogCancer… pic.twitter.com/2dgEhC8uCf
“Parkinson’s disease is the fastest-growing neurological condition on the planet,” notes neurologist Dr. Michael Okun, echoing what countless clinics witness daily: rising diagnoses, earlier onsets, and families scrambling for answers. Motor symptoms tremor, rigidity, slowness often steal the spotlight, but non-motor changes such as anxiety, sleep disruption, and cognitive fog quietly erode a person’s sense of self just as profoundly.
Crucially, while current medications can replenish dopamine or smooth a shaking hand, they do not plug the leak that keeps draining the well. The real enemy is the relentless march of those misfolded proteins from cell to cell an invisible relay race that medicine has struggled to stop.
Understanding this silent struggle does more than deepen empathy; it sets the stage for a radical new approach. If we can interrupt the very handshake that lets toxic alpha-synuclein slip through neuronal doorways, we may shift from merely treating symptoms to arresting the disease’s advance itself. The discovery that follows is not just a scientific milestone it’s a reason for millions to imagine movement, memory, and identity reclaimed.
How a Protein Spreads Destruction
Every mystery has a culprit and in Parkinson’s disease, it wears a familiar name: alpha-synuclein. It’s a protein found in every healthy brain, quietly helping neurons communicate. But when it misfolds, it turns from helpful to harmful like a trusted guide suddenly leading travelers off a cliff.
These misfolded forms of alpha-synuclein don’t just stay where they are. They clump together into sticky aggregates and move from neuron to neuron, spreading toxicity like a whisper that becomes a wildfire. This chain reaction transforms healthy proteins into rogue ones, overwhelming brain cells and ultimately killing them. The result? A slow, unforgiving loss of the very cells responsible for movement, emotion, and thought.
Scientists now know this spread isn’t random. Like a virus needing a host, these toxic proteins need an entry point a way to slip past the cell’s defenses. And here’s where the story deepens.
Recent research has identified two crucial doormen: Lag3 and Aplp1. These proteins sit on the surface of neurons, acting like receptors or access gates. Alone, they each enable the misfolded alpha-synuclein to enter. But together, they supercharge the process, dramatically increasing the amount of toxic protein absorbed by brain cells.
Think of them as accomplices: one unlocks the door, the other pulls the villain inside.
Once inside, the damage escalates. These clumps hijack the cell’s machinery, cause inflammation, disrupt energy production, and eventually lead to a specific kind of programmed cell death a process called parthanatos. This death isn’t chaotic it’s orchestrated, precise, and devastating.
The spread of alpha-synuclein is what drives Parkinson’s progression. It’s why symptoms worsen over time, and why the disease can jump from motor to cognitive regions of the brain. It’s not just the loss of dopamine it’s the contagious nature of this misfolded protein that lies at the heart of the illness.
What Scientists Discovered About Two Proteins
Sometimes the biggest answers hide in plain sight. For years, researchers suspected that the misfolded alpha-synuclein proteins fueling Parkinson’s disease weren’t working alone. They needed help an accomplice inside the cell’s gates. And now, they’ve found it. Or rather, two of them.
Meet Aplp1 and Lag3 proteins once quietly doing their jobs on the surface of neurons, now thrust into the spotlight as key players in the spread of Parkinson’s. Each of these proteins can bind to toxic alpha-synuclein. Each can help usher it into healthy brain cells. But what scientists at Johns Hopkins discovered is far more consequential: when Aplp1 and Lag3 work together, they become a powerful conduit one that significantly accelerates the uptake and internal spread of the toxic protein.
In a series of precise and elegant experiments, researchers showed that deleting either Aplp1 or Lag3 in mice slowed down the progression of Parkinson’s-like symptoms. But when both were removed, something extraordinary happened over 90% of the disease-related transmission and neurotoxicity was blocked. Not only were the toxic clumps unable to spread, but dopamine-producing neurons were preserved, and behavioral symptoms vanished.
Digging deeper, scientists identified a specific seven-amino acid stretch a kind of molecular “handshake” shared by both proteins that allowed them to bind with alpha-synuclein. Remove that, and the transmission chain breaks. Even more compelling? This Aplp1-Lag3 complex doesn’t just promote binding; it also drives the toxic protein deep into cells via a process called endocytosis essentially, it invites the enemy inside and closes the door behind it.
But this breakthrough didn’t stop at genetic deletions. Researchers used an antibody originally developed to treat cancer by targeting Lag3 to block the Aplp1-Lag3 interaction. The result? The toxic spread was stopped, neurodegeneration was halted, and motor function in mice was preserved.
It’s a breathtaking discovery. What once seemed like a slow and inevitable decline in Parkinson’s may now have a choke point, a place we can intervene. And this choke point isn’t theoretical it’s targetable, right now, with a drug that’s already FDA-approved for another disease.
The Promise of a Repurposed Drug

Breakthroughs in medicine don’t always start from scratch. Sometimes, they come from seeing an old tool in a new light. In this case, the tool is a cancer drug. The light? Hope for millions living with Parkinson’s disease.
The same antibody drug that helps treat melanoma nivolumab/relatlimab, already approved by the FDA has now been shown to block the toxic partnership between Aplp1 and Lag3. And in doing so, it stops something once thought unstoppable: the spread of Parkinson’s disease within the brain.
Here’s what the researchers found: when this drug, which was originally developed to help the immune system recognize and destroy tumors, was administered to mice with Parkinson’s-like pathology, the results were profound. It prevented toxic alpha-synuclein clumps from entering neurons, preserved dopamine-producing brain cells, reduced motor dysfunction, and halted the progression of brain damage. In some cases, the effects were even stronger than removing both Aplp1 and Lag3 genetically.
That’s because the antibody doesn’t just stop the disease at the cellular level it reaches deep into the mechanism of transmission itself. By binding to the D3 domain of Lag3 the exact spot where Aplp1 interacts it severs the handshake that allows toxic proteins to be absorbed by healthy cells. And when that handshake is broken, the chain of destruction is cut short.
Even more encouraging? The drug successfully crossed the blood-brain barrier, a notorious gatekeeper that often blocks therapies from reaching the brain. That means this isn’t just a test tube fantasy it’s a real-world possibility.
What makes this so promising isn’t only the science it’s the timeline. Because the drug is already approved and known to be safe for human use, the path to clinical trials for Parkinson’s patients could be dramatically accelerated. This isn’t decades away. This is something we can act on now.
And the implications reach further still. Since Lag3 has also been implicated in Alzheimer’s disease and other conditions involving protein misfolding, this approach could open new doors in the fight against multiple neurodegenerative diseases.
A New Era of Hope for Millions
Hope can feel like a fragile thing especially for those living with Parkinson’s disease. It’s a condition that doesn’t just disrupt the body it slowly rewrites identity. Every lost gesture, forgotten word, or stumbled step becomes a quiet grief. And until now, treatments could offer relief, but not reprieve. Progress felt inevitable. Irreversible.
But this breakthrough changes the narrative. By revealing how alpha-synuclein spreads its damage through the handshake between Aplp1 and Lag3 scientists have found a vulnerable link in the disease’s armor. And by using an already-approved cancer drug to block that link, they’ve shown we don’t need to start from scratch to stop this disease in its tracks.
This matters not just because it’s scientifically elegant but because it’s actionable. It means that millions of people around the world those living with Parkinson’s now and those yet to be diagnosed could one day have a way to slow or even stop the march of symptoms.
It matters for every caregiver watching a loved one disappear in slow motion.
For every patient wondering how much longer they’ll be able to write, walk, or speak.
For every doctor searching for something more than a temporary fix.
This discovery is more than a medical milestone. It’s a shift in perspective from managing decline to reclaiming possibility.
Where Do We Go From Here?
Science may move in data and detail, but its destination is deeply human. This discovery the disruption of the Aplp1-Lag3 partnership and the potential to repurpose a cancer drug to halt Parkinson’s marks more than a clinical achievement. It’s a spark of momentum in a field long overshadowed by uncertainty.
But we must remember: this is not the finish line. It’s the beginning of a new direction.
While the results in mice are inspiring, human brains are more complex. Clinical trials will be essential. Questions remain about long-term effects, about safety in people with varying stages of Parkinson’s, about how early this treatment must be applied to make a difference. Hope must be paired with patience, and breakthroughs with rigorous testing.
Yet something has already changed: the very possibility that we can intervene at the root of this disease. That we may no longer be limited to treating symptoms while watching the storm advance. That maybe, for the first time, we can disarm the storm itself.
As we look ahead, this moment challenges us scientists, doctors, patients, and loved ones alike not just to wait, but to participate. Support research. Stay informed. Share what’s unfolding. Because every step forward is accelerated by the voices that demand better, by the minds that dare to believe in more.
The journey to healing may be long, but today, it feels a little more possible than yesterday.
Loading...

