New Drug That Protects the Blood-Brain Barrier Shows Promise Against Alzheimer’s Disease
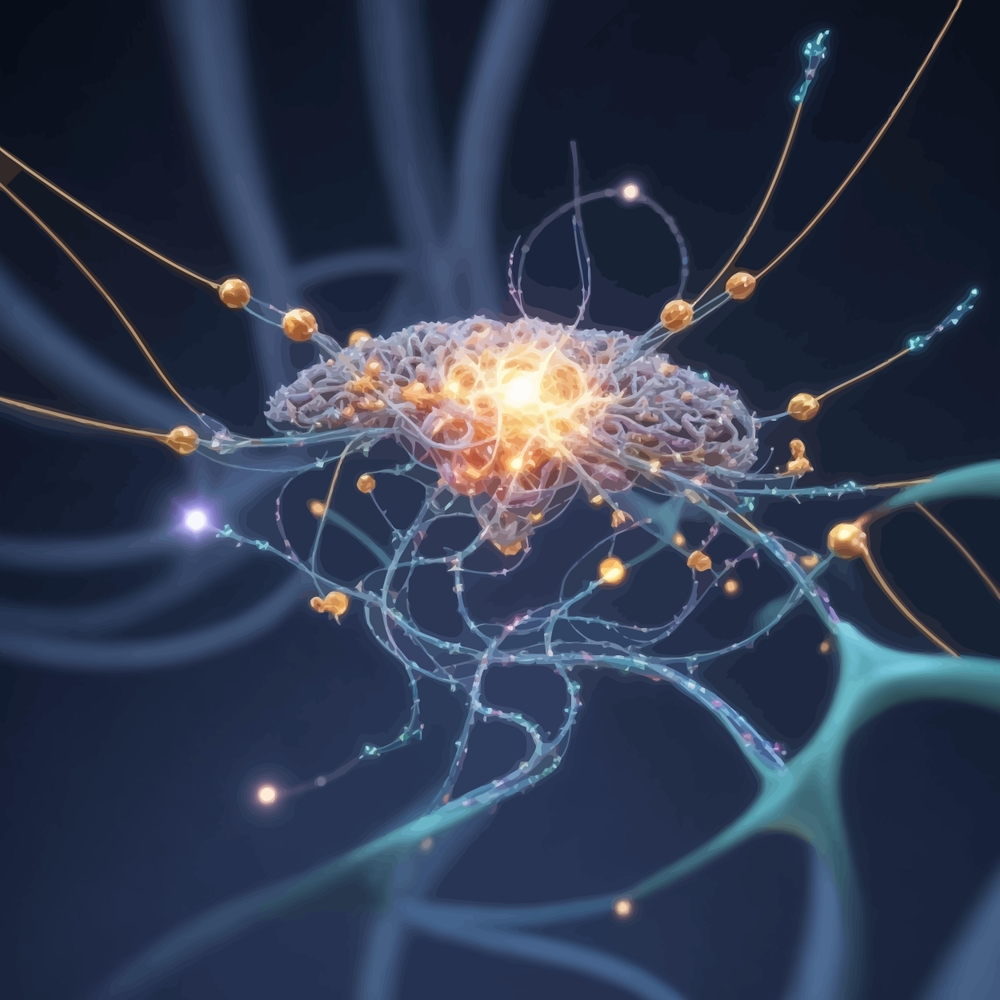
Imagine your brain as a walled city vibrant, intelligent, alive. Inside, billions of neurons fire like the hum of electricity in a bustling metropolis. But this city has a gatekeeper: a near-invisible shield known as the blood-brain barrier. It’s the silent protector, deciding who enters and who stays out. And when that shield starts to crack, chaos isn’t far behind.
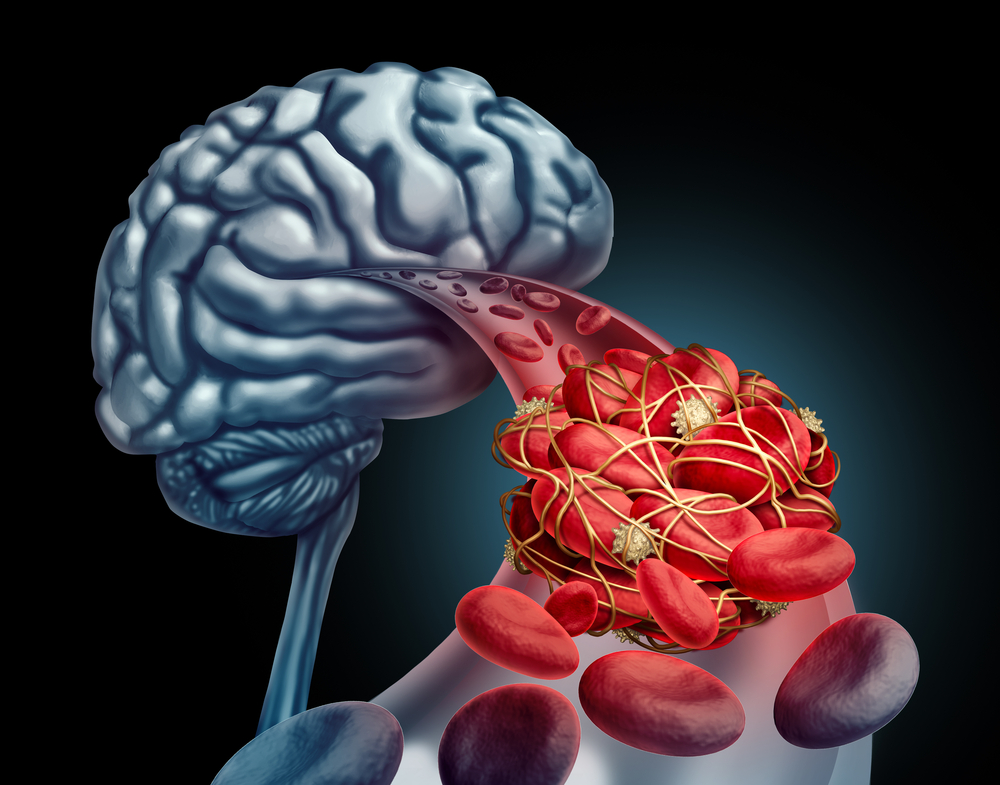
Over 55 million people worldwide live with dementia, most of them with Alzheimer’s disease. For decades, science has chased one main culprit: amyloid plaques clumps of protein that pile up in the brain and disrupt communication. Entire treatments have been designed to scrub them away. But what if plaques are only part of the story? What if the real danger begins before they even form at the breakdown of the brain’s natural defenses?
Recent breakthroughs suggest a surprising new direction in Alzheimer’s research. Rather than fighting the damage after it’s done, scientists are now looking at how to stop it at the source by protecting the blood-brain barrier. And at the center of this discovery is a drug that doesn’t target plaques at all. It targets the barrier itself.
This shift may not just redefine how we treat Alzheimer’s it could change how we think about the disease entirely.
Rethinking the Battlefield
For years, the dominant narrative in Alzheimer’s research has revolved around amyloid plaques sticky accumulations of protein that form between neurons and disrupt communication. These plaques became the chief suspects in the disease’s progression, and so, the battle lines were drawn. Drug after drug was designed to clear them, including gantenerumab, a monoclonal antibody that binds to amyloid and signals the immune system to remove it.
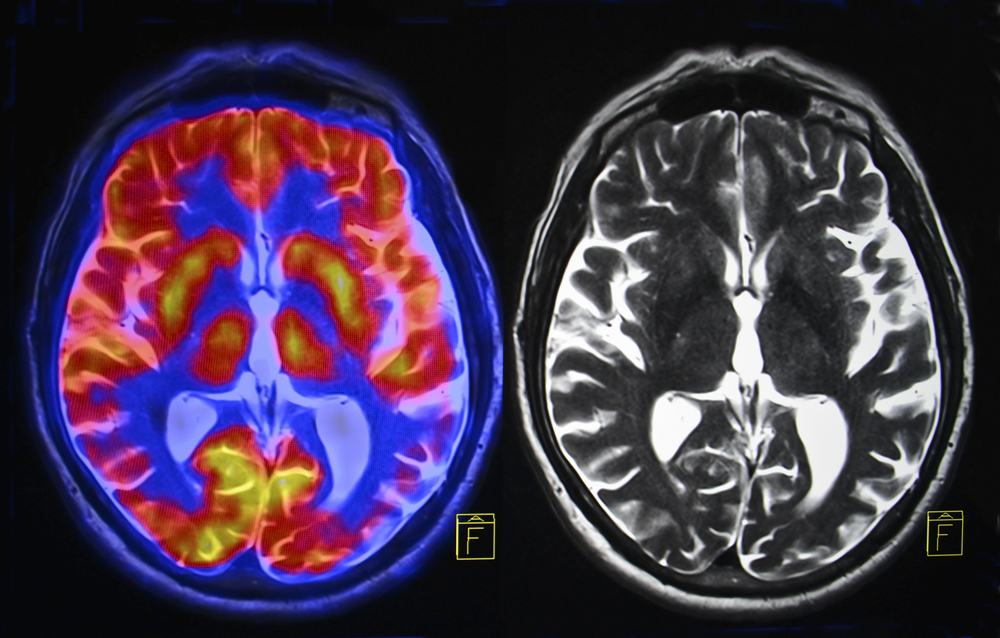
On paper, the approach made sense. And to some extent, it worked. Gantenerumab, for example, showed the ability to reduce amyloid buildup in the brains of people with early-onset Alzheimer’s, especially those with genetic mutations that almost guarantee the disease. In a small subgroup of individuals treated over several years, the drug cut the risk of developing symptoms in half. Brain scans confirmed a drop in amyloid levels.
But there was a catch and it was a big one. The cognitive benefits were modest, and side effects were common. Over half the participants experienced amyloid-related imaging abnormalities, including brain swelling and microbleeds. These issues raised concern about the safety and long-term viability of such treatments. And despite promising early data, gantenerumab was eventually pulled from development due to insufficient overall clinical benefit.
This pattern isn’t unique. Similar drugs donanemab, lecanemab have shown some plaque-clearing ability but delivered inconsistent or limited cognitive improvements. The cost is high, the outcomes are uncertain, and the risks remain significant.
These results have forced researchers to step back and reconsider the central dogma. If clearing plaques doesn’t consistently restore memory or halt decline, perhaps plaques aren’t the root cause or at least not the only one. This realization is turning scientific attention away from fighting what’s already broken, and toward understanding why the damage begins.
What the Blood-Brain Barrier Really Does
The brain is the body’s most complex organ and its most protected. Shielding it is the blood-brain barrier (BBB), a tightly woven layer of specialized cells that functions like a customs checkpoint. It carefully filters what enters the brain from the bloodstream, allowing in vital nutrients and oxygen while keeping out toxins, bacteria, and harmful immune cells.
In a healthy brain, this barrier operates silently and efficiently. But when it starts to break down as research increasingly shows it does in Alzheimer’s disease its failure sets off a chain reaction of damage. Inflammatory proteins, free radicals, and unwanted immune cells seep into brain tissue. The result is swelling, oxidative stress, and the slow death of neurons. The hippocampus the brain’s memory hub is particularly vulnerable to this assault.
What’s striking is how early this breakdown can occur. In both humans and animal models, BBB deterioration has been observed before significant amyloid buildup or memory loss. That changes the narrative. It suggests that Alzheimer’s might not just be a disease of protein plaques, but of a breached defense system that allows those plaques and other toxic processes to take hold in the first place.
Importantly, BBB failure isn’t unique to Alzheimer’s. It’s seen in aging, traumatic brain injuries, and other neurodegenerative disorders. This makes the BBB a common denominator in many forms of cognitive decline and an appealing target for new therapies.
Until recently, most Alzheimer’s treatments overlooked the barrier entirely. But as one study after another reveals its role in early disease progression, that’s changing. Preserving the integrity of the BBB doesn’t just slow damage it could prevent it. It’s not about sealing the brain off completely, but about protecting the inner environment where brain cells thrive.
The Role of 15-PGDH in Brain Damage
Deep within the cells that line the blood-brain barrier is an enzyme with a complicated name and a destructive role: 15-hydroxyprostaglandin dehydrogenase, or 15-PGDH. Under normal conditions, this enzyme helps regulate inflammation by breaking down certain signaling molecules. But in the aging brain and in Alzheimer’s something goes wrong. 15-PGDH activity ramps up, and instead of maintaining balance, it begins to dismantle the brain’s defenses from within.
Researchers have found elevated levels of 15-PGDH in both mice and humans affected by neurodegeneration, particularly in microglia and perivascular macrophages immune cells that are tightly connected to the brain’s blood vessels. When overactivated, this enzyme degrades molecules that help reduce inflammation and support the structural integrity of the BBB. The result? A weakened, more permeable barrier that can no longer keep harmful agents out.
This process creates a vicious cycle. As the barrier degrades, it allows more inflammatory substances into the brain, which in turn triggers even more 15-PGDH activity. That feedback loop accelerates damage, making the brain increasingly vulnerable to the very forces it was designed to resist.
To break this cycle, scientists developed SW033291, a compound designed to block 15-PGDH. Originally studied for its potential in tissue regeneration, the drug has found a new and promising application: protecting the blood-brain barrier in neurodegenerative conditions.
In preclinical studies, the results were remarkable. Mice treated with SW033291 showed preserved memory and cognitive function even in the presence of amyloid plaques. Their blood-brain barriers remained intact. Inflammatory damage was reduced. And perhaps most notably, the treatment didn’t touch the amyloid levels at all. That’s a critical detail it means the drug works through an entirely different pathway than traditional Alzheimer’s treatments.
Even more promising is the drug’s potential beyond Alzheimer’s. In models of traumatic brain injury, a major risk factor for dementia, SW033291 prevented memory loss and neurodegeneration when administered within 24 hours of injury. That broad utility makes 15-PGDH a compelling target not just for treatment, but for prevention.
As clinical trials begin to move this compound from mice to humans, the scientific community is watching closely. If results hold up, SW033291 could mark the beginning of a new era in brain health one focused not on undoing damage, but on reinforcing the brain’s natural resilience.
How SW033291 Could Change the Game
Boosting enzyme in brain immune cells could help treat Alzheimer's disease
— Dr Singularity (@Dr_Singularity) August 6, 2025
Cedars-Sinai researchers found that boosting the enzyme ACE in brain immune cells (microglia) protected mice against Alzheimer’s disease.
Using gene editing, they enhanced ACE in microglia, restoring… pic.twitter.com/vYzcZxyYSC
Unlike traditional Alzheimer’s drugs, which focus on reducing amyloid buildup, SW033291 works by blocking the enzyme 15-PGDH, which undermines the blood-brain barrier (BBB). By inhibiting this enzyme, the drug preserves the protective integrity of the barrier keeping toxins, inflammatory molecules, and immune cells out of the brain’s fragile environment.
In Alzheimer’s mouse models, the impact was profound. Mice treated with SW033291 retained their cognitive function and memory. Their brains showed no signs of the typical inflammation, neuron loss, or BBB damage that usually marks the disease’s progression. Even in the presence of amyloid plaques, the brain’s defensive shield remained intact and that protection translated into preserved function.
What makes this especially important is that SW033291’s effects are completely independent of amyloid reduction. This sets it apart from nearly every other Alzheimer’s drug currently available or in development. It challenges a decades-old assumption in neurology: that amyloid is the main driver of decline, and that clearing it is the only path to treatment. Instead, it suggests that if you keep the brain’s environment stable if you protect what protects the brain you may not need to remove the plaques at all to maintain cognitive health.
The drug’s potential doesn’t stop at Alzheimer’s. In studies involving traumatic brain injury (TBI) another condition that compromises the BBB – SW033291 was equally effective. Given just 24 hours after injury, the drug prevented memory loss and neurodegeneration in mice. That kind of broad-spectrum neuroprotection hints at a future where the same treatment might help not just those at risk of dementia, but people recovering from concussion, stroke, or age-related cognitive decline.
Mechanistically, SW033291 preserves molecules that are critical to the brain’s resilience anti-inflammatory lipid mediators and neuroprotective prostaglandins that 15-PGDH would otherwise destroy. By maintaining these protective compounds, the drug keeps the BBB strong and the inflammatory cascade in check.
Early safety data from animal studies are encouraging, but clinical trials in humans are the necessary next step. They will determine dosage, long-term effects, and how this treatment performs in real-world settings. But the concept itself a drug that stabilizes the brain’s defenses without trying to reverse the damage represents a powerful shift in strategy.
Protecting Your Brain Starts Now
While SW033291 is still in preclinical stages and not yet available for human use, its focus on preserving the blood-brain barrier (BBB) offers practical insight. The BBB doesn’t collapse overnight. It weakens gradually chipped away by aging, poor lifestyle choices, chronic inflammation, and trauma. That means we have a window of opportunity. And the choices we make each day can help keep this critical shield strong. Here’s what the research points to:
- Prioritize Deep, Restorative Sleep
Sleep isn’t just rest it’s repair. During deep sleep, the brain flushes out waste products and reduces inflammation. Chronic sleep deprivation has been linked to increased BBB permeability and higher Alzheimer’s risk. Protecting your sleep is protecting your brain. - Control Blood Pressure and Blood Sugar
High blood pressure and type 2 diabetes damage small blood vessels, including those that form the BBB. Keeping cardiovascular and metabolic health in check is essential for maintaining barrier integrity. - Fight Chronic Inflammation
Inflammation is a slow, silent saboteur of brain health. Diets high in processed foods, sugar, and unhealthy fats increase inflammatory markers that weaken the BBB. In contrast, anti-inflammatory foods like leafy greens, berries, fatty fish, olive oil, and turmeric support long-term brain resilience. - Protect Your Head
Even mild concussions can compromise the BBB. Whether you’re on a bike, in a car, or playing a contact sport, take your brain seriously. Helmets, seatbelts, and simple precautions can help avoid trauma that may have long-term cognitive consequences. - Exercise Regularly
Physical activity improves blood flow to the brain, reduces oxidative stress, and enhances the production of protective molecules. Regular movement keeps the BBB robust and your mind sharper for longer. - Limit Alcohol and Avoid Smoking
Both impair BBB function and increase the brain’s exposure to toxins. Reducing or eliminating these habits lowers your risk not only for dementia, but for a range of chronic diseases.
These aren’t shortcuts, they’re commitments. Small, sustained habits that guard the brain’s border and buy precious time in the fight against neurodegeneration. They echo the same philosophy behind SW033291: protect the system early, and you may not have to fix it later.
Guardians of the Mind
For decades, Alzheimer’s research chased the visible amyloid plaques, memory loss, neuron death while one of the brain’s most essential protectors stayed in the background. But now, the blood-brain barrier is stepping into the spotlight, not as a passive structure, but as a powerful gatekeeper of cognitive health.
The discovery that a single enzyme, 15-PGDH, can weaken this barrier and accelerate brain damage and that blocking it with SW033291 can preserve memory even in the presence of amyloid signals a turning point. It challenges long-held assumptions and offers a fresh strategy: prevent the damage before it begins.
This shift isn’t just scientific it’s philosophical. It reminds us that healing doesn’t always mean fighting harder. Sometimes, it means reinforcing what’s already there. Strengthening the brain’s natural defenses, supporting its environment, and valuing the subtle systems that quietly sustain life.
We’re still early in this journey. SW033291 must prove itself in human trials. But the direction is clear: the path forward in Alzheimer’s may not lie in simply clearing what goes wrong but in protecting what’s right.
And perhaps the most hopeful part? You’re not waiting on the sidelines. Your daily habits, your lifestyle choices, your attention to sleep, stress, food, and movement they all shape the health of that invisible shield. Science may deliver the breakthroughs, but you still hold the frontline.
Loading...

