China’s New Bio-Patch Heals Organs Without Surgery No Scalpel, No Stitches, Just Regeneration

Imagine healing a damaged heart without a single incision—no scalpel, no stitches, no hospital stay. Just a paper-thin patch, placed gently on the surface of an organ, quietly doing what medicine has long dreamed of: helping the body regenerate itself.
For decades, treating internal organs has meant navigating a maze of complexity. Surgeons must cut through layers to reach the target, while medications take the long route through the bloodstream—often with limited precision and unwanted side effects. But what if we could bypass all that?
Chinese researchers may have done just that. In a stunning leap for regenerative medicine, they’ve developed a bio-patch that adheres directly to organs, delivering therapeutic drugs with pinpoint accuracy and helping tissue repair itself from the inside out. It’s thinner than a band-aid, smarter than a pill, and powerful enough to change how we treat some of the most life-threatening conditions.
At its core, this innovation is more than a medical device—it’s a shift in how we think about healing. And the story of how it works, and what it could mean for the future of surgery-free medicine, is as fascinating as the science itself.
The Challenge of Healing Dynamic Organs
Treating organs like the heart, lungs, or intestines isn’t just a medical challenge—it’s an engineering dilemma. These “dynamic” organs are in constant motion. The heart beats over 100,000 times a day, lungs expand and contract with every breath, and intestines shift continuously during digestion. This relentless activity makes it incredibly difficult to apply traditional therapeutic materials like surgical patches or implants. Anything too rigid risks tearing delicate tissue. Anything too soft might not hold up.
The complexity runs deeper. These organs aren’t uniformly structured. Their tissues are anisotropic, meaning their physical properties vary depending on direction—like wood grain or muscle fibers. They also have auxetic behaviors, expanding in width when stretched, which is rare in natural or synthetic materials. That combination of multi-directional strain and irregular architecture creates a biomechanical environment that most medical materials simply weren’t built to handle.
Traditional surgical interventions come with their own complications: trauma from incisions, risk of infection, long recovery times, and the possibility that the repair won’t last. Even advanced regenerative patches have struggled. Most are isotropic—designed with uniform properties in every direction—and can’t stretch, bend, or breathe the way living tissue does. When applied to a beating heart or expanding lung, these conventional materials may peel off, fail to integrate, or stress the surrounding tissue, undermining healing efforts.
What Is China’s Bio-Patch?
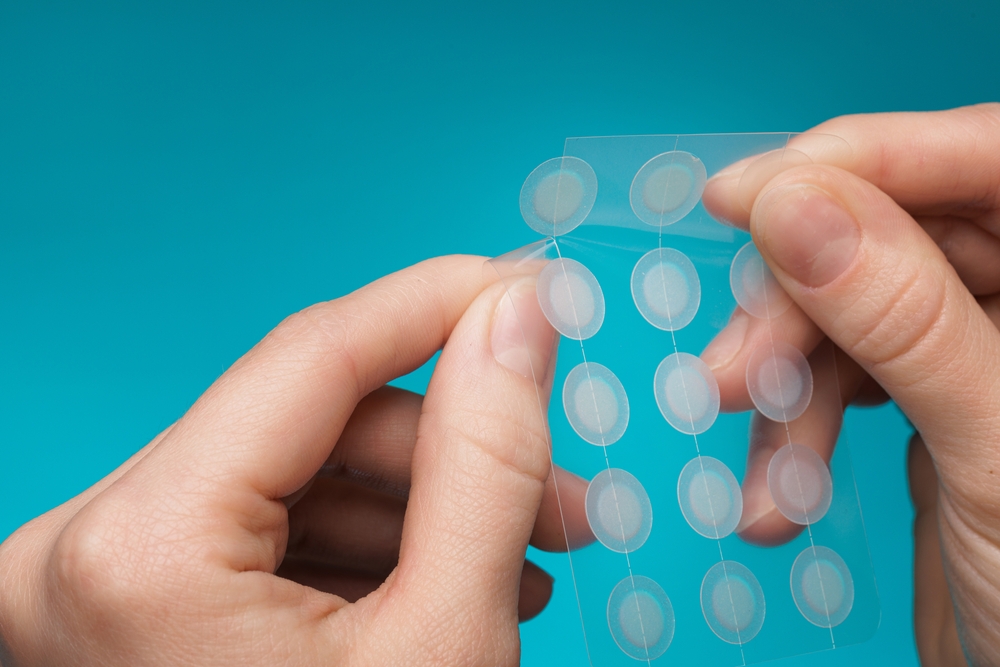
At first glance, it resembles nothing more than a transparent film—thin, flexible, almost weightless. But China’s new bio-patch is a marvel of medical engineering, designed to adhere to the surface of internal organs and deliver life-saving treatments directly where they’re needed, without surgery.
Developed through a collaboration between researchers at institutions like Beihang University and Peking University, the NanoFLUID bio-patch combines nanotechnology, bioelectronics, and regenerative medicine into one sophisticated platform. It’s chipless, battery-free, and incredibly precise. Once applied—either under the skin or directly to an organ—it uses wireless power to activate tiny internal components that release drugs into surrounding tissues, bypassing the body’s traditional drug delivery systems entirely.
What sets this patch apart isn’t just its form factor—it’s how it works on a cellular level. The patch contains nano-scale channels and microelectrodes that generate ultra-high electric fields. These fields create safe, temporary pores in nearby cell membranes, a process called electroperforation, allowing medications to enter cells rapidly and effectively. In fact, this method has been shown to be over 100 times faster than traditional diffusion-based drug delivery.
And despite its high-tech mechanisms, the patch is fully biocompatible. Made from soft, flexible materials, it conforms easily to organ surfaces without causing irritation or damage. It requires no incisions, no wired implants, and no onboard electronics, reducing the risk of infection and making it far easier to use than previous generations of implantable devices.
Already tested in preclinical models, the patch has successfully treated breast tumors, acute liver injury, and delivered gene-editing materials directly to target tissues. But its true promise lies in its potential flexibility: because the patch is programmable and adaptable, it could be used to treat a wide range of conditions, from cancer to autoimmune diseases, with pinpoint accuracy.
Why This Technology Is a Game-Changer

What makes China’s bio-patch more than just another medical device is its potential to rewrite the rules of organ treatment. For decades, the standard model has remained largely unchanged: diagnose the problem, treat the entire body, and hope enough of the drug reaches the target organ to make a difference. This shotgun approach often demands higher doses, increasing the risk of side effects, while offering only marginal gains in precision. The bio-patch flips that model on its head.
Direct-to-organ therapy—the core advantage of the patch—means medicine no longer has to take the long road through the bloodstream, facing dilution and degradation. Instead, treatments can be delivered exactly where they’re needed, at the cellular level, in controlled doses. This radical efficiency not only boosts effectiveness but also reduces collateral damage to healthy tissues. In conditions like cancer, where powerful drugs often wreak havoc on the immune system and vital organs, this level of precision could dramatically reduce patient suffering.
Then there’s the non-invasive nature of the patch. Traditional surgical interventions, even minimally invasive ones, come with risks: bleeding, infection, scarring, and long recovery periods. This patch, however, is applied without cutting or stitching. It adheres naturally to the organ, forming a stable interface that can remain functional without the need for sutures—thanks in part to materials inspired by nature, such as tree-frog pads and microneedle architectures. This makes it not only safer but potentially far more accessible in outpatient or emergency settings.
Equally groundbreaking is the adaptive architecture of the patch. Unlike rigid devices, it’s designed to move with the organ. Whether it’s expanding with the bladder, contracting with the heart, or stretching across a breathing lung, the patch flexes and shifts in tandem with its biological host. Its anisotropic and auxetic properties make this possible—engineering terms that, in essence, mean the patch mirrors the very movements and mechanical complexity of the tissue it’s meant to heal.
Finally, this bio-patch isn’t limited to drug delivery. Its modular design means it could be adapted to deliver gene therapies, immune-modulating agents, or even regenerative biologics like stem-cell-derived exosomes. This opens the door to future applications such as preventing transplant rejection, accelerating wound healing, or even reversing chronic disease progression in situ.
The Science Behind the Patch
Healing an organ isn’t just about delivering drugs—it’s about creating the right environment for cells to recover, regenerate, and function as part of a living, moving system. That’s the central engineering challenge this new bio-patch tackles head-on: how do you build a material that not only delivers therapy but also becomes part of the body’s natural mechanics?
The answer lies in biomimicry—the science of designing materials that replicate the structures and behaviors of living tissues. Dynamic organs like the heart, lungs, and intestines are not only in constant motion, but they also possess complex internal architectures. Their fibers, cells, and extracellular matrix are aligned in specific directions, a property called anisotropy. For instance, cardiac muscle fibers contract more efficiently in one direction than another, a design that’s essential for pumping blood efficiently.
The patch reproduces this by incorporating directional patterns and fiber alignments that match the native tissue. This anisotropy allows it to “speak the same mechanical language” as the organ, ensuring better integration and function. But that’s only half the equation.

Dynamic organs also expand and contract simultaneously in multiple directions—a rare mechanical behavior known as auxeticity. Most materials, when stretched, become thinner; auxetic materials, by contrast, become wider. This unusual trait is common in soft tissues like the heart, lungs, and bladder, allowing them to withstand and recover from large deformations without damage. The bio-patch uses auxetic architectures—like re-entrant honeycombs and sinusoidal lattices—to mimic this behavior. These microstructures allow the patch to expand and contract in sync with the tissue, reducing mechanical stress and improving durability.
To achieve this delicate balance of strength, flexibility, and biocompatibility, scientists use advanced materials like electroconductive hydrogels, silk fibroin, polylactic acid (PLA), and PEG-based polymers. These materials are layered or 3D-printed into microscale lattices and infused with functional agents—from drugs to stem cells. In some cases, multi-material printing and hybrid fabrication methods are used to integrate vascular channels, allowing the patch to nourish the regenerating tissue and support cell survival.
Some versions of the patch are even electrically active, enabling synchronized cell signaling in electrically sensitive tissues like the heart. Others are embedded with biologic payloads, such as growth factors or exosomes, to promote cell repair and immune modulation.
Early Results and Future Potential

In one study, researchers applied the patch to treat breast tumors in mice. Unlike traditional chemotherapy, which circulates broadly through the body and harms healthy cells along the way, the patch delivered anti-cancer agents directly to the tumor site. This localized delivery significantly reduced tumor size while minimizing systemic toxicity—an early validation of its promise in oncology.
Another breakthrough came in models of acute liver injury, a condition notoriously difficult to manage due to the liver’s delicate, rapidly changing tissue environment. The patch adhered securely to the organ and delivered therapeutic agents that helped suppress inflammation and accelerate repair. These findings are critical: they suggest that even organs with high regenerative capacity, like the liver, can benefit from targeted, non-invasive support when under severe stress.
But perhaps most exciting is the patch’s potential for gene editing and advanced diagnostics. Researchers have used it to deliver CRISPR-based materials directly into cells, opening doors for treating genetic conditions that were previously out of reach for systemic therapies. In one experiment, the patch was used to identify DUS2, a key driver in lung-specific cancer metastasis—showing how it could serve not only as a treatment device but also as a diagnostic tool that helps uncover disease mechanisms in real time.
These results—while limited to animal models for now—point toward a future where a single, non-invasive patch could replace or complement entire treatment protocols. Imagine applying a patch to a transplanted organ to release anti-rejection drugs, reducing the need for lifelong immunosuppression. Or delivering stem-cell-derived factors to regenerate damaged heart tissue after a heart attack. Or using the patch as a “smart dressing” for internal wounds, releasing anti-inflammatory agents and promoting cellular healing in situ.
Of course, several hurdles remain. Human trials will be necessary to validate safety, durability, and effectiveness. The patch’s long-term biocompatibility, scalability, and regulatory path will determine how quickly it can be adopted in clinical settings. But with its non-invasive application, precise control, and regenerative capabilities, the patch stands out as a truly versatile platform—not just for one disease, but for a broad spectrum of medical needs.
Ethical, Safety, and Accessibility Considerations

A central concern is biocompatibility. While early animal studies suggest the patch can integrate well with tissue and degrade safely over time, human physiology introduces far more variables. Long-term implantation—especially on constantly moving organs—raises questions: Will the patch maintain integrity under the strain of years of contractions or inflammation? Could it cause scarring, immune reactions, or interfere with neighboring tissues? Ensuring the patch doesn’t disrupt normal organ function will require extended safety trials and post-market surveillance once it reaches clinical use.
Equally critical is the electroperforation process the patch uses to deliver drugs or gene-editing agents. While the electric fields involved are low-amplitude and designed to avoid damage, any interaction with cellular membranes must be stringently monitored for unintended effects—especially when delivering potent therapies like CRISPR or anti-cancer agents. Regulators will need to evaluate not just therapeutic outcomes, but the precision and reversibility of the patch’s intracellular access.
Then there are ethical implications, particularly with gene-editing applications. If the patch allows localized delivery of genome-modifying materials, what safeguards will ensure its use is confined to therapeutic—and not enhancement—purposes? And who decides what constitutes appropriate use when gene therapy is involved? These questions will demand proactive guidelines, transparent consent processes, and thoughtful public engagement.
On a practical level, scalability and accessibility may be among the biggest barriers to global impact. The patch’s fabrication—requiring high-resolution printing, smart materials, and sometimes patient-specific customization—might initially drive up costs. Without strategies to streamline production or subsidize access, there’s a risk the patch becomes available only in elite research hospitals or well-funded health systems, further widening health disparities.
And finally, there’s the matter of training and infrastructure. While the patch is designed to be minimally invasive, applying it to internal organs may still require specialized techniques—potentially involving endoscopic tools, imaging guidance, or robotic assistance. Healthcare systems, especially in low-resource settings, may need support to adopt these tools safely and effectively.
A Step Toward Truly Personalized, Non-Invasive Medicine
The advent of China’s bio-patch signals more than a medical breakthrough—it reflects a broader evolution in how we approach healing itself. Medicine is moving steadily away from one-size-fits-all treatments and invasive procedures, toward precision interventions that are tailored, targeted, and as gentle as they are effective. The bio-patch exemplifies this shift: a smart, adaptable platform that delivers treatment not through force, but through finesse.
What makes this moment especially significant is the convergence of disciplines that made it possible. Material science, bioelectronics, regenerative biology, and nanotechnology are no longer operating in isolation. Instead, they’re coming together to create solutions that feel almost intuitive—tools that integrate seamlessly with the body’s own rhythms. The bio-patch doesn’t just treat disease; it learns from tissue mechanics, mimics natural functions, and assists healing in a way that respects the body’s complexity rather than overwhelming it.
This personalized approach extends beyond mechanical compatibility. Imagine patches infused with a patient’s own stem cells, releasing custom-formulated therapies on demand, guided by sensors that monitor inflammation or healing progress in real time. As AI and computational modeling improve, future versions of the patch could be designed not just for a disease, but for your disease—factoring in your organ shape, movement patterns, cellular environment, and genetic profile.
Moreover, because the patch is non-invasive and adaptable, it opens doors for earlier intervention and broader access. Instead of waiting until surgery becomes the only option, clinicians could apply a patch in outpatient settings to support organ repair before irreversible damage occurs. It also holds promise for low-resource environments, where advanced surgical care may be limited but non-invasive, self-powered therapeutics could still be deployed.
Of course, challenges remain. But the path forward is clear: by combining high-precision engineering with biologically informed design, medicine can move from reactive to proactive, from invasive to integrative. The bio-patch may be one small device, but its implications ripple outward—toward a future where healing feels more natural, more personal, and far less painful.
In that vision, the scalpel is no longer the symbol of medical progress. Instead, it’s a sliver of soft material, placed delicately on the surface of a beating heart, doing its quiet work without a cut or a stitch—just regeneration.
Loading...

