Scientists Just Removed HIV From Human Immune Cells Using Crispr Gene Editing

Imagine if a few rogue sentences were buried deep in the story of your life—sentences you didn’t write, but that quietly shaped everything: your health, your choices, your future. Now imagine there was finally a way to edit them out—cleanly, precisely, and for good.
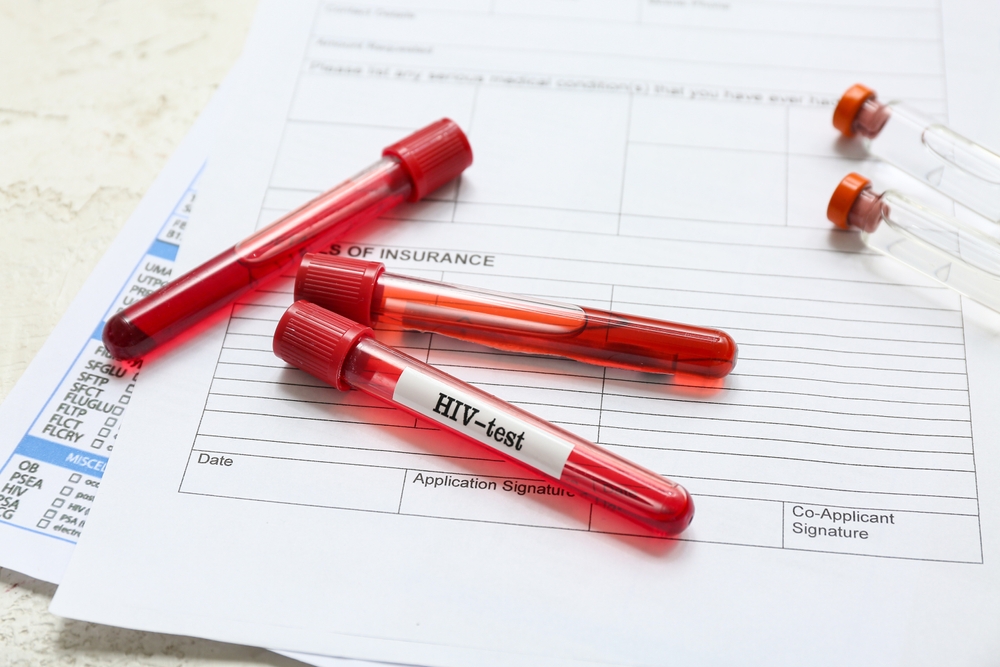
For over 40 years, HIV has been one of those sentences. Not just a virus, but a shadow etched into the DNA of more than 38 million people worldwide. We’ve learned how to silence it, to keep it quiet with daily pills and fierce determination. But we’ve never been able to remove it—until now.
With a single injection and a technology once thought to be science fiction, researchers have just done what was once unthinkable: they removed a virus from the genetic code of living cells. Not suppressed. Not stalled. Removed.
So what does this mean for the future of HIV—and for all of us?
The Silent War Within
HIV doesn’t just infect the body—it infiltrates the blueprint of life itself. Unlike most viruses that come and go, HIV is a master of disguise. Once inside, it doesn’t float in the bloodstream waiting to be attacked. It hides. It embeds its genetic material into the DNA of human immune cells—particularly CD4+ T cells, the very soldiers meant to protect us. From there, it lies dormant, untouched by even the most powerful drugs. A sleeper agent, waiting.
This is why, despite the life-saving power of antiretroviral therapy (ART), a cure has remained out of reach. ART can suppress the virus so low it’s undetectable, but it can’t reach these hidden reservoirs. And if someone stops treatment? The virus doesn’t hesitate—it awakens, replicates, and reclaims ground like a fire reigniting in dry grass.
Scientists have said HIV can successfully be removed from infected cells, using Crispr gene-editing technology. pic.twitter.com/W41Pxpsd2O
— Naija (@Naija_PR) March 20, 2024
Scientists call these hidden pockets “latent reservoirs.” They’re scattered throughout the body: in the blood, the brain, the lymph nodes, the spleen. Some researchers have found that even when a person’s blood shows no sign of active virus, there can still be over 100 million cells silently harboring HIV’s genetic blueprint. That’s the haunting reality—HIV isn’t just managed; it’s embedded.
Even more puzzling is the case of “repliclones”—clusters of infected cells that multiply, copy after copy, passing the virus along like a secret family heirloom. These clones can persist for years, churning out small amounts of virus despite daily medication. They don’t play by the rules, and they don’t go down easily.
For millions of people, this hidden war isn’t just biological—it’s psychological. It’s the burden of a fight that doesn’t end. The pills, the stigma, the waiting for the next breakthrough.
The Molecular Scalpel Changing Everything
For generations, we’ve fought viruses with blunt instruments—vaccines, pills, and hope. But what if we could go deeper, straight to the source, and edit out the virus like a typo in a manuscript?
Enter CRISPR.
CRISPR isn’t a drug. It’s not a bandage or a suppressant. It’s a tool—small, precise, and powerful. Think of it as a pair of molecular scissors guided by a microscopic GPS. Originally discovered as a bacterial defense mechanism against invading viruses, CRISPR has now become one of the most revolutionary technologies in modern medicine. Its mission? To seek and destroy unwanted genetic code.
In the context of HIV, CRISPR doesn’t just target the virus floating in the blood. It homes in on the infected cells where HIV has embedded itself—hiding inside the DNA, like graffiti on the walls of your genetic house. CRISPR can recognize these viral blueprints and cut them out, potentially leaving behind a cell that’s virus-free.
This isn’t theoretical. It’s already happening in labs and now, remarkably, in living beings. Researchers have used CRISPR to remove SIV—a close relative of HIV—from the DNA of monkeys, in a way that was not only effective but safe. No off-target damage. No chaos in the genetic code. Just precision.
That precision matters. HIV mutates quickly and hides deeply. But CRISPR’s ability to use “guide RNAs”—like address labels—means scientists can now direct it to multiple regions of the viral genome simultaneously. That makes it harder for the virus to escape. It’s like locking all the exits before removing an intruder.
And here’s the most profound part: it only took a single injection to set all this in motion.
Removing HIV from Immune Cells
In 2024, something extraordinary happened. After decades of fighting HIV with external defenses—pills, treatments, protocols—scientists went internal. They went into the very code of infected immune cells and cut the virus out.
At Temple University’s Lewis Katz School of Medicine, a team led by Dr. Kamel Khalili and Dr. Tricia Burdo developed a CRISPR-based treatment called EBT-001. They tested it on rhesus macaques infected with SIV, the monkey version of HIV. The results were more than promising—they were historic.
With just a single intravenous injection, EBT-001 traveled throughout the body, reaching the deepest viral reservoirs: the lymph nodes, spleen, blood, and even the brain. Once inside, the CRISPR system located the SIV DNA hidden in immune cells and sliced it out with surgical precision. And most astonishing of all—it did this without harming the surrounding genetic code. No toxicity. No off-target chaos. Just clean removal of the virus, like erasing the wrong sentence from a book without tearing the page.
Animals who received the higher dose didn’t just survive—they thrived. Some even gained weight and showed improved immune function compared to the untreated group. The treatment was safe, well-tolerated, and effective. And for the first time, scientists witnessed widespread in vivo gene editing of a virus embedded in living tissue—not in a dish, not in theory, but in the living body.
This breakthrough paved the way for the next step: human trials.
The FDA approved the launch of a clinical trial for EBT-101, a version of the CRISPR therapy designed to target HIV in humans. Delivered through a harmless virus (AAV9), EBT-101 uses multiple guide RNAs to strike three separate regions of the HIV genome at once—closing off escape routes and aiming to permanently inactivate the virus.
Why Curing HIV Is So Hard
Hope is rising—but so are the questions. If we can now remove HIV from infected cells, why haven’t we cured it yet? Why does the fight still feel so uphill?
The truth is, HIV doesn’t just infect—it embeds, it replicates, it hides. And it does so in ways that have kept even our most advanced therapies chasing shadows.
One of the biggest obstacles is the existence of latent reservoirs. These are cells—primarily resting CD4+ T cells—that harbor integrated HIV DNA but don’t actively produce the virus. They lie in wait, silent and invisible to the immune system and to antiretroviral drugs. These cells can live for decades, and if ART is stopped, they can wake up and reignite the infection like a spark to dry timber.
Then there are the repliclones—cells that don’t just contain the virus but make copies of themselves, spreading HIV’s genetic imprint even under treatment. It’s like trying to drain a lake while invisible springs keep filling it from beneath.
Even when CRISPR works—when it edits the virus out of certain cells—the challenge remains: how do you find and reach every last infected cell? HIV can hide in the brain, in the lymph nodes, in tissues we’re only beginning to understand. Missing even a few can allow the virus to return.
There’s also the issue of delivery. Getting CRISPR to the right cells, in the right tissues, without triggering immune reactions or damaging healthy DNA, is a complex balancing act. While adeno-associated viruses (like AAV9) have proven to be safe carriers so far, ensuring consistent and widespread delivery in humans is a mountain we’re still climbing.
And let’s not forget mutation. HIV is notorious for its ability to evolve. If we target one site in its genome, it can escape through another. That’s why EBT-101 targets three distinct regions of the virus simultaneously—to close the escape hatches before the virus can slip away.
Finally, there’s the scale. A person with undetectable HIV levels may still carry tens of millions of infected cells. Removing every single one—without harming the host—is like defusing bombs scattered across a battlefield, each buried under layers of camouflage.
Hope Meets Science

The breakthroughs with CRISPR aren’t just about HIV. They’re the first steps in a broader revolution—one where we don’t just treat symptoms or hold diseases at bay. We go to the root. We rewrite what’s been written.
Researchers are already exploring how CRISPR can tackle other persistent viruses like herpes and hepatitis B, or even correct genetic disorders that were once considered lifelong burdens. We’re entering an era where healing may no longer mean management—but erasure.
But this progress isn’t just measured in petri dishes or clinical trials—it lives in the hearts of those who’ve waited for decades. People who’ve taken their medications every day, who’ve endured side effects, stigma, silence. For them, this science means something deeper: it means possibility.
Still, the work ahead is steep. Clinical trials take time. Questions of access, ethics, and equity must be faced head-on. A cure that only reaches a few isn’t a cure—it’s a privilege. We must demand that these technologies serve humanity as a whole, not just those who can afford them.
But let’s not miss what’s happening here. The walls that HIV once built—walls of fear, of permanence, of biological imprisonment—are beginning to crack. And through those cracks, light is pouring in.
The Power to Rewrite Our Stories
Somewhere inside each of us is a story we didn’t choose.
Maybe it’s an illness. A wound. A memory. Maybe it’s a virus written into our very cells. For too long, HIV has been one of those stories—a silent line etched deep into the lives of millions, dictating who they could love, how they lived, and what they feared.
But here’s the truth science is now teaching us: no story is final.
CRISPR isn’t just a tool of science—it’s a metaphor for something far greater. The power to edit. To remove what harms. To reclaim what was lost. To say, “This isn’t how my story ends,” and then make that true.
Yes, we are still early in this journey. There are challenges ahead, and not every question has been answered. But we’ve stepped into a new chapter—one written not in fear, but in fierce, informed hope.
So whether you’re someone living with HIV, someone carrying another kind of pain, or someone simply watching from the sidelines—this moment is an invitation. To believe in healing. To support the science that brings it closer. And to remember that even the deepest scars in our DNA do not define who we are.
They are not the end of the sentence.
They are the place where we pick up the pen.
Because when we embrace the power to rewrite our stories—through science, through spirit, through solidarity—we don’t just change our own lives.
We begin to change the world.
Loading...

