Study Shows No Evidence That Depression Is Caused by a Chemical Imbalance in the Brain
For decades, depression has been explained as a chemical imbalance in the brain, a theory that suggests low serotonin levels are the root cause. It’s an idea that has shaped not only how doctors treat depression but also how society understands mental health. The appeal of this explanation is clear—it’s simple, medical, and seemingly fixable with the right pill.
But what if this theory is flawed?
Recent research has challenged the serotonin imbalance model, showing no solid evidence that depression is caused by a lack of serotonin. Instead, scientists are uncovering a far more complex reality, one that involves brain structure, genetics, inflammation, and life experiences. This shift in understanding is more than just academic—it changes everything about how we approach mental health and treatment.
If depression isn’t just about serotonin, what’s really going on? And more importantly, what does this mean for those struggling to find relief?
Debunking the Chemical Imbalance Theory

The idea that depression is caused by a chemical imbalance—specifically, low serotonin—originated in the 1960s and gained momentum in the 1990s with the rise of selective serotonin reuptake inhibitors (SSRIs). Pharmaceutical ads reinforced this notion, presenting depression as a straightforward issue of brain chemistry that medication could correct. It was a simple, reassuring explanation. But science has since revealed that this theory doesn’t hold up.
Comprehensive reviews and meta-analyses have failed to find consistent evidence linking serotonin levels to depression. Some studies show no difference in serotonin activity between depressed and non-depressed individuals, while others suggest that antidepressants work through mechanisms beyond serotonin regulation. If low serotonin were the cause, SSRIs should work for everyone—but they don’t. Many people don’t respond to these medications, and some improve with treatments that don’t affect serotonin at all.
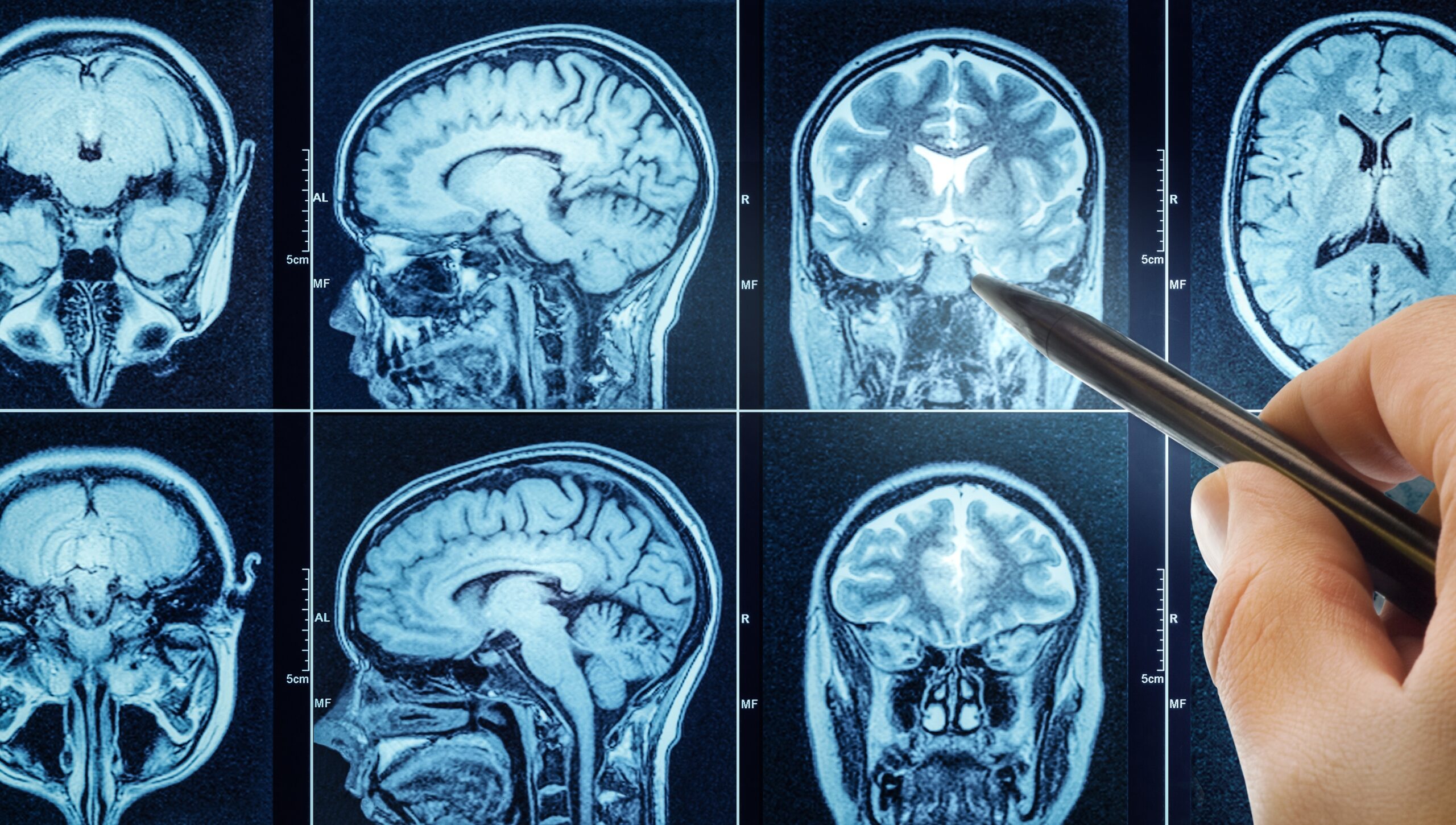
Brain imaging studies further challenge the serotonin hypothesis. Researchers have found no distinct serotonin patterns that separate those with depression from healthy individuals. Instead, depression appears to involve multiple brain circuits, genetic factors, and external influences. The chemical imbalance theory, once widely accepted, has been largely debunked. Now, scientists are shifting their focus to a more complex and holistic understanding of what really causes depression.
What Recent Research Really Says About Depression
If serotonin isn’t the root cause of depression, then what is? Recent research paints a far more complex picture, showing that depression is influenced by multiple biological and environmental factors rather than a single chemical imbalance.
Advanced imaging studies, including PET and fMRI scans, have found no consistent differences in serotonin levels between people with and without depression. Genetic studies have also failed to establish a clear link between serotonin-related genes and the condition. Meanwhile, antidepressants that increase serotonin don’t work for everyone, and their delayed effects—often taking weeks—suggest that serotonin alone isn’t responsible for mood regulation. If depression were just about fixing a neurotransmitter imbalance, relief would come much faster.
Beyond serotonin, researchers are now looking at other biological processes, such as inflammation and brain structure changes. Some studies have found that people with depression have increased levels of inflammatory markers, suggesting a connection between chronic stress, immune responses, and mental health. Others have identified changes in brain regions like the hippocampus and prefrontal cortex, which play key roles in mood, memory, and decision-making. These findings suggest that depression is not a simple neurotransmitter issue but a condition shaped by a complex interplay of brain function, genetics, and life experiences.
Biological and Psychological Factors in Depression

Depression isn’t just about brain chemistry—it’s deeply influenced by thoughts, experiences, and the world around us. While biological factors contribute, research shows that psychological and environmental influences are just as crucial in shaping mental health.
Biological Influences
- Brain structure and function: Neuroimaging studies reveal that individuals with depression often have a smaller hippocampus, a brain region crucial for memory and emotional regulation. Chronic stress can shrink this area, making emotional resilience more difficult.
- Inflammation and immune response: Studies show elevated inflammatory markers in people with depression, suggesting a link between chronic stress, immune function, and mood disorders. Some researchers are now exploring anti-inflammatory treatments as potential interventions.
Psychological and Environmental Influences
- Cognitive patterns: Persistent negative thinking, self-criticism, and cognitive distortions can reinforce depression, creating a cycle that is difficult to break. Cognitive Behavioral Therapy (CBT) has been effective in addressing these patterns.
- Life events and stress: Trauma, financial struggles, grief, and major life changes are common depression triggers. The way individuals process and cope with these events plays a crucial role in their mental health.
- Social connection: Loneliness and isolation are among the strongest predictors of depression. People with strong support systems tend to recover more effectively, while those lacking social bonds are at higher risk for prolonged symptoms.
Depression isn’t just a biological glitch—it’s a condition shaped by the interaction of the brain, mind, and environment. Acknowledging this complexity is key to finding better ways to heal.
How These Findings Affect Treatment Approaches

The outdated idea of a chemical imbalance led to treatment strategies focused almost entirely on correcting serotonin levels. But as research uncovers a more complex picture of depression, treatment approaches are evolving beyond just medication.
Expanding Pharmacological Options
- Beyond SSRIs: While selective serotonin reuptake inhibitors (SSRIs) remain widely used, their limitations have led researchers to explore alternative medications. Treatments targeting the glutamate system, such as ketamine, have shown promise in providing faster relief for some individuals.
- Anti-Inflammatory approaches: Given the link between inflammation and depression, some studies suggest that anti-inflammatory drugs may help certain patients, though more research is needed.
The Importance of Therapy and Mindset Shifts
- Cognitive Behavioral Therapy (CBT): Since thought patterns play a crucial role in depression, CBT helps individuals challenge negative thinking and develop healthier mental habits.
- Mindfulness and stress management: Meditation, mindfulness practices, and stress-reduction techniques are increasingly recognized for their role in improving mood and resilience.
Lifestyle Interventions
- Exercise and brain health: Regular physical activity has been shown to reduce symptoms of depression, likely due to its effects on brain chemistry and stress reduction.
- Sleep and nutrition: Poor sleep and an unbalanced diet can worsen depressive symptoms. Prioritizing restorative sleep and nutrient-rich foods can support overall mental well-being.
The Multidisciplinary Approach
- Personalized treatment plans: Effective care involves a combination of medication (if needed), therapy, lifestyle adjustments, and social support. A one-size-fits-all approach no longer makes sense in light of what we now understand about depression.
- Community and support networks: Healing isn’t just about medical interventions—it’s about connection. Strengthening social bonds and engaging in supportive communities can have a profound impact on recovery.
Moving beyond the outdated serotonin model opens the door to more effective, holistic treatments that address the full picture of depression. The more we understand, the better we can tailor solutions that truly help people heal.
Rethinking Depression and the Path to Healing
For years, depression was framed as a simple serotonin imbalance—a message that shaped treatments, public perception, and even how people saw themselves. But science tells a different story. Depression isn’t just about brain chemistry; it’s influenced by brain structure, stress, inflammation, life experiences, and even the way we think.
This doesn’t mean hope is lost—it means hope is bigger than we thought. It means that struggling with depression isn’t a sign of personal weakness or a broken brain. It means healing can come in many forms, whether through therapy, lifestyle changes, meaningful connections, or emerging treatments that go beyond outdated models. No one should feel trapped by a theory that no longer holds up when real, effective paths to healing exist.
Depression is complex, but that’s not a reason to despair—it’s a reason to explore. It’s a call to look beyond old narratives and embrace a broader, more holistic approach to mental health. Understanding depression in its full depth doesn’t just change how we treat it—it changes how we support each other, how we heal, and how we move forward.
Featured Image Source: Shutterstock
Sources:
- Moncrieff, J., Cooper, R. E., Stockmann, T., Amendola, S., Hengartner, M. P., & Horowitz, M. A. (2022). The serotonin theory of depression: a systematic umbrella review of the evidence. Molecular Psychiatry, 28(8), 3243–3256. https://doi.org/10.1038/s41380-022-01661-0
- Jauhar, S., Cowen, P. J., & Browning, M. (2023). Fifty years on: Serotonin and depression. Journal of Psychopharmacology, 37(3), 237–241. https://doi.org/10.1177/02698811231161813
Loading...