Experts Sound Alarm as Drug-Resistant Fungus Attacking Groin and Bum Rises at Frightening Pace

A concerning new health alert is spreading across the UK as experts warn that a so called super fungus is moving quickly through communities and proving extremely difficult to treat with standard medication. The infection is caused by Trichophyton indotineae, a newly identified dermatophyte species that has emerged from the Indian subcontinent in what studies describe as a near epidemic form. According to experts quoted across recent reports, the fungus is now spreading into the UK at a pace that has surprised clinicians and raised questions about how prepared national health systems are for drug resistant fungal diseases.
What began as a rare and largely unfamiliar condition in Britain has surged into a significant medical talking point as cases have reportedly risen by almost 500 percent in the last three years. The UK National Mycology Reference Laboratory has found that the fungus now accounts for 38 percent of dermatophyte isolates sent in for testing. Experts explain that many of these isolates display resistance to terbinafine, a commonly used NHS fungal treatment, meaning patients are often left struggling with persistent symptoms and long courses of more potent medication that can carry serious side effects. With warnings that infections could soon seep into the wider population, public health specialists say awareness is an essential first line of defence.
Drug-resistant 'super fungus' that attacks groin and bum spreading through UK and can be transmitted by sex https://t.co/YVXCOuRljy pic.twitter.com/pAOZqmavvY
— Daily Star (@dailystar) November 25, 2025
The Rise Of A Fast Spreading Infection
The first major red flag surrounding Trichophyton indotineae is its rapid rise in areas where it was previously almost undocumented. According to reports, infections in the UK and Ireland climbed from 44 before 2022 to 258 by March of this year. Experts at a conference in Poland expressed concern at this trajectory and emphasised that this pattern shows no indication of slowing. Professor Darius Armstrong James, a fungal expert at Imperial College London, warned that infections are “becoming a really big problem in the UK” and that the growing number of cases appearing in hospitals is “very concerning”. His comments highlight the unpredictability of novel fungal strains that adapt quickly and spread efficiently.
Many of the patients affected in the UK so far are people of South Asian heritage, which experts believe is linked to travel and higher exposure in regions where the fungus is already established. However Dr David Denning from the University of Manchester cautioned that this pattern is unlikely to remain contained. He explained that it “won’t be long” before infections appear more widely across the population and added that “this is clearly going to become a big issue across the world”. These statements underline concerns that once a resistant fungal species gains momentum it can embed itself into community transmission with surprising speed.
The organism thrives in warm and moist environments and spreads through direct skin contact or contaminated surfaces. Because of this, healthcare specialists believe it may spread more silently than expected. The fact that it emerged quietly before multiplying so sharply indicates how easily fungal infections can go unnoticed until they reach a tipping point in population data.
This is a groin fungal infection (jock itch). It is very stubborn and difficult to treat. Most people have been treating it for years. But why is that so?
— Riley (@RileyTrades1) March 31, 2025
~ Open thread 🧵 pic.twitter.com/5aGIipcrCn
Why Trichophyton Indotineae Is Hard To Treat
This infection has attracted attention partly because it resists terbinafine, the medication most commonly prescribed through the NHS for ringworm and related infections. Laboratory testing has shown that many isolates do not respond to the drug, and the reference articles confirm that “most infections are clinically resistant to it”. This level of resistance forces doctors to move patients to itraconazole, a stronger antifungal that often requires months of treatment and carries risks such as liver damage or heart problems.
The American Academy of Dermatology Association has stated that the condition has emerged within the last decade and mutated over the years to become increasingly robust. This mutation is what has led to the nickname super fungus. According to reports, this development allows the organism to withstand a range of standard treatments and remain active on skin for extended periods. Patients whose symptoms fail to improve with over the counter creams frequently experience frustration and confusion before receiving an accurate diagnosis that explains the persistence of the rash.
The increased reliance on itraconazole also brings new challenges. Because the drug demands long treatment windows, doctors must monitor patients for harmful reactions while ensuring adherence. The process can be exhausting for patients whose symptoms cause pain, irritation, and embarrassment. These realities demonstrate why experts believe the situation must be taken seriously even though case numbers remain relatively low.

Image Credit: Shutterstock
Symptoms That Should Not Be Ignored
Trichophyton indotineae usually targets the groin, thighs, and buttocks, creating red, itchy rashes that sufferers describe as painful and extremely uncomfortable. According to both reference articles, the rash appears in ring shaped patterns with raised scaly borders and can expand outward if not treated. These rashes are often referred to as angry or formidable because of their intensity and persistence. If left untreated the infection can spread to the back, face, and other areas, increasing the likelihood of scarring and secondary infection.
One of the most problematic aspects is that the condition can be mistaken for eczema or psoriasis. Professor Armstrong James pointed out that it “could be easily mistaken for eczema or psoriasis if tests are not conducted”. GP Megha Pancholi added that eczema is not infectious and does not spread through contact, whereas T. indotineae passes easily between people or via contaminated fabrics. She also explained that “using a corticosteroid cream may in fact worsen symptoms” because steroids suppress the skin’s immune response and give the fungus more room to grow.
These factors often delay proper diagnosis. Individuals may treat what they assume is eczema only to find their symptoms intensifying. This misunderstanding increases transmission risk because the infected person may continue regular contact with others without realising the cause of their discomfort.
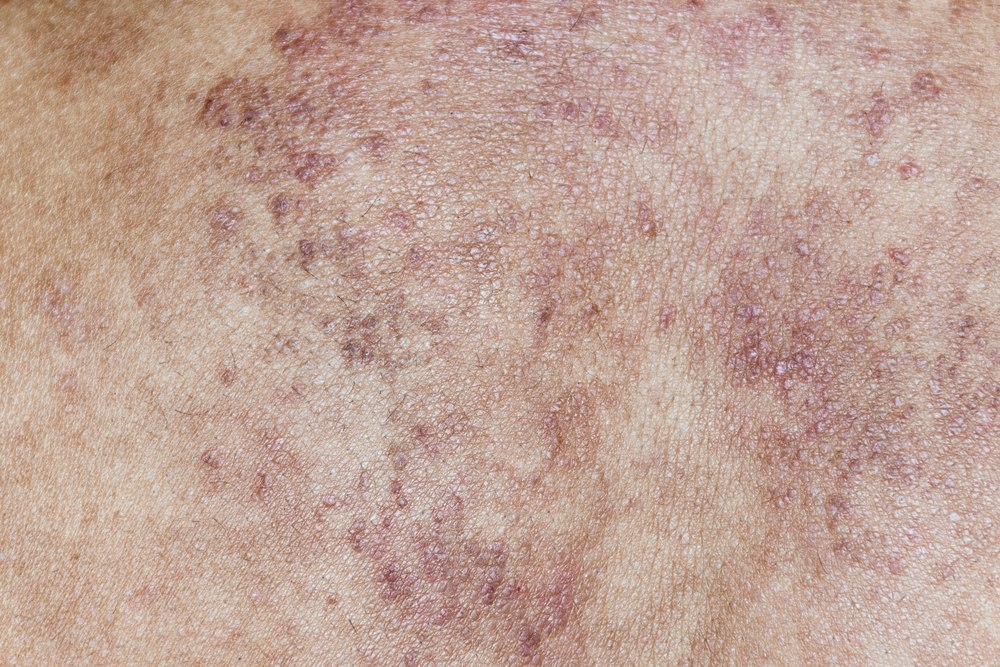
Image Credit: Shutterstock
Why Experts Are Sounding The Alarm
Beyond the physical symptoms, the infection carries a heavy social burden. Dr Denning stated that “it is very socially limiting” and explained that sufferers may feel unable to leave their homes or attend work. He added that people can “become social pariahs” because of the stigma and discomfort associated with visible rashes in sensitive areas. These consequences extend beyond medicine into wellbeing, confidence, and mental health.
As the reports emphasise, the ease of person to person spread is a major concern. Shared towels, clothing, bedding, or gym equipment can all transfer the fungus, and environments that remain warm or damp give it an ideal habitat. Experts say that once a fungus with these characteristics becomes established, community outbreaks become much harder to contain. The fact that several isolates in vitro are resistant to terbinafine only intensifies this risk.
Public health specialists fear that the infection’s ability to hide in plain sight, combined with misdiagnosis, could allow it to move through communities more widely than current numbers show. With increased global travel and climatic conditions that favour fungal infections, experts believe vigilance is essential.

Image Credit: Shutterstock
If You Suspect Symptoms What You Should Do
GP Megha Pancholi advises that anyone who notices burning or itchy rashes around the groin, thighs, or buttocks should see a GP immediately. She warns that symptoms are unlikely to improve with over the counter prescriptions, so medical evaluation is crucial. Early testing helps distinguish the infection from eczema or other skin conditions and ensures that the correct antifungal treatment is prescribed.
Doctors typically require patients to complete the full course of antifungal medication even if symptoms begin to subside. This reduces the risk of recurrence and prevents further resistance from developing. Because itraconazole can cause liver or heart related side effects, healthcare providers may need to perform follow up checks.
To avoid spreading the infection Dr Pancholi recommends keeping lesions covered, avoiding shared items such as towels and bedding, and washing these items above 60°C. She also emphasised maintaining good personal hygiene and regular handwashing. These measures significantly lower the risk of transmission in households or communal settings.
Image Credit: Shutterstock
A Reminder Of Our Changing Health Landscape
The rise of this drug resistant super fungus highlights an important truth about modern health challenges. Microorganisms continue to evolve and adapt, sometimes faster than our treatments can keep up. While case numbers remain relatively low the rapid growth rate and resistance patterns demonstrate why experts are urging increased awareness.
This story offers a reminder that early diagnosis, careful hygiene practices, and public education remain essential tools in managing emerging infections. By paying close attention to symptoms and seeking medical help promptly individuals can protect themselves and others. The situation also underscores the need for continued research into antifungal resistance as healthcare systems prepare for future challenges.
Staying informed and responsive allows communities to remain resilient even as unfamiliar threats emerge.
Featured Image credit: Shutterstock
Loading...

