Gene Therapy Breakthrough Offers Hope as Huntington’s Disease Progression Slowed by 75%

For the first time in history, scientists have achieved a major breakthrough in the fight against Huntington’s disease. In a groundbreaking gene therapy trial, researchers have successfully slowed the progression of this fatal neurodegenerative disorder by an astonishing seventy-five percent. This finding represents not only a leap forward in genetics but also a triumph of human determination over one of nature’s cruelest inherited fates.
The achievement comes after decades of tireless research, countless failed trials, and immense dedication from global scientific teams determined to decode one of medicine’s most complex genetic puzzles. Huntington’s disease, often described as a blend of Alzheimer’s, Parkinson’s, and ALS combined, has challenged researchers for generations. Scientists have worked relentlessly to understand how one mutated gene could wreak such widespread havoc on the brain and nervous system.
What makes this breakthrough particularly remarkable is the spirit of collaboration behind it. The success story is built on an unprecedented partnership between neuroscientists, geneticists, and clinical specialists who united to target the disease at its molecular core. Laboratories across continents shared data, expertise, and patient insights, accelerating progress that once seemed impossible. This teamwork proved that when science unites with compassion, the results can transform lives.
A Historic Milestone in Neuroscience
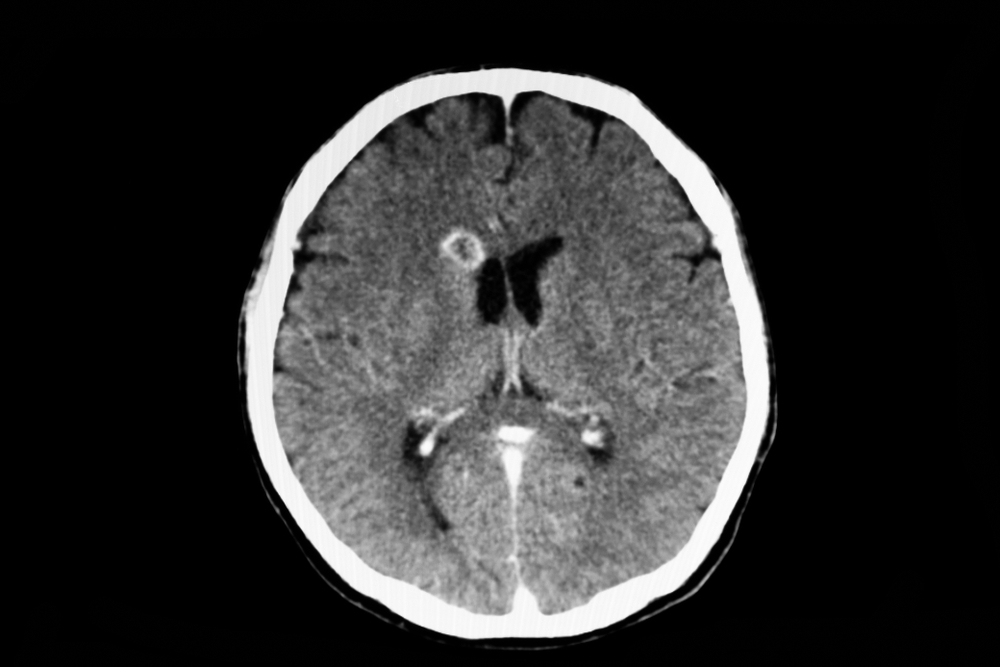
Huntington’s disease has long been one of the most devastating hereditary disorders known to science. Caused by a defective gene that produces a toxic protein, it leads to the gradual breakdown of nerve cells in the brain. Patients experience uncontrolled movements, cognitive decline, and severe psychiatric symptoms. Most tragically, there has never been a cure or even an effective treatment that could slow its relentless progression.
That has now changed. According to research published and reported by The Guardian and BBC News, the world’s first gene therapy targeting the root cause of Huntington’s has shown extraordinary results. The experimental treatment, known as AMT-130, uses a modified virus to deliver a healthy copy of the gene to brain cells, effectively silencing the faulty one.
This milestone did not emerge overnight. It is the result of decades of cumulative knowledge built from earlier genetic studies, animal models, and patient-led advocacy that pushed the scientific community to explore the impossible. Researchers had to overcome extraordinary barriers, including developing techniques to safely deliver genetic material into delicate brain tissues. Each small success laid the groundwork for this defining moment, demonstrating the power of persistence in scientific innovation.
The success of this trial has also ignited renewed energy across the neuroscience community. Universities and biotech firms are already collaborating to refine the therapy, expand clinical trials, and explore how the same approach might apply to other neurodegenerative diseases. What was once an unreachable goal now serves as a blueprint for future genetic medicine, inspiring hope not only for Huntington’s patients but for anyone battling a hereditary neurological condition.
How the Treatment Works
The gene therapy was developed by the biotechnology company uniQure and tested in collaboration with major research institutions across Europe and the United States. Unlike conventional medications that only manage symptoms, this therapy targets the genetic source of the disease.
Here is how it functions:
- Delivery System: Scientists use a harmless adeno-associated virus to carry therapeutic genetic material into brain cells.
- Gene Silencing: Once inside, the therapy instructs neurons to produce small RNA molecules that suppress the production of the toxic mutant huntingtin protein.
- Sustained Effect: Because neurons are long-lived, the effect could potentially last for many years, making this a one-time treatment rather than a lifelong regimen.
In the latest clinical trial, patients who received the treatment showed a seventy-five percent reduction in disease progression compared with those receiving standard care. Some even reported improvements in motor coordination and mood regulation within months.

A Lifeline for Families Living with Huntington’s
For families who have watched generation after generation suffer from Huntington’s disease, this breakthrough feels nothing short of miraculous. The disease affects roughly one in every ten thousand people worldwide, though its impact ripples far beyond those diagnosed. Each child of an affected parent has a fifty percent chance of inheriting the faulty gene, creating an atmosphere of fear and uncertainty for entire family trees.
For many, the news of this treatment has brought an overwhelming sense of relief and gratitude. Families who once lived in constant anxiety about genetic test results are beginning to imagine futures filled with possibility instead of fear. Parents who carried the gene can finally hope that their children may grow up free from the same fate that defined generations before them.
Communities affected by Huntington’s are also beginning to reconnect with optimism. Support groups, advocacy organizations, and medical researchers have all expressed that this breakthrough feels like the first step toward a new chapter, one defined not by despair but by determination. The collective sense of empowerment is growing, inspiring more people to participate in research and spread awareness about the importance of genetic science in transforming human lives.

The Broader Scientific Impact
Beyond Huntington’s disease, the success of this gene therapy opens doors to a new era of personalized medicine. For decades, scientists have dreamed of curing diseases by correcting the underlying genetic code. Now, that vision is beginning to take shape.
Gene therapies have already shown promise in treating blood disorders like sickle cell anemia and certain types of blindness. Yet, neurological conditions have been notoriously difficult to treat due to the complexity of the brain and the challenge of delivering treatments past the blood-brain barrier.
This trial proves that it can be done. It demonstrates that gene therapy can safely and effectively reach deep brain regions, opening the possibility for future cures for Alzheimer’s, Parkinson’s, and ALS.
The ripple effects of this achievement extend far beyond neurology. It provides researchers with a working model for designing future genetic interventions across a range of diseases once thought untreatable. By mapping how viral vectors interact with brain tissue and understanding immune responses, scientists can adapt these findings to make gene therapy safer and more precise. This success is teaching the scientific world invaluable lessons about how to translate genetic theory into life-saving practice.
Challenges and Cautions Ahead
While the results are groundbreaking, scientists urge cautious optimism. This was an early-phase trial, and larger studies are still needed to confirm long-term safety and efficacy. There are also challenges in manufacturing and distributing such therapies, which can cost hundreds of thousands of dollars per treatment.
Researchers are also investigating potential side effects. Although none of the trial participants experienced severe adverse reactions, gene therapy involves altering the genetic expression of cells, a step that must be monitored over time for any unexpected consequences.
Another important consideration lies in ensuring equitable access to this revolutionary treatment. Many experts warn that without global cooperation and public health planning, such advanced therapies could remain available only to the wealthiest patients or nations. Bridging that gap will require policies that promote affordability, transparency, and open data sharing between medical institutions worldwide.
There is also the long-term responsibility of monitoring how these genetic modifications behave over decades. Scientists will need to track treated individuals to ensure the therapy remains safe and effective as they age. These follow-up studies could provide valuable insights that shape the future of gene editing and help fine-tune similar approaches for other diseases.

What This Means for the Future of Medicine
If gene therapies continue to succeed, the future of healthcare could shift from symptom management to true biological repair. The idea that doctors could one day cure genetic diseases rather than merely treating their effects represents a paradigm shift in modern medicine.
Over the next decade, researchers plan to explore similar therapies for other inherited disorders. Efforts are already underway to adapt this technology for conditions such as spinal muscular atrophy, Tay-Sachs disease, and certain forms of epilepsy.
It also raises profound ethical and social questions. How will healthcare systems manage the cost of such advanced treatments? Will insurance cover them? And what will this mean for populations in low-income countries? These are challenges the global medical community will have to navigate as the science continues to advance.
Feature image by Vitaly Gariev | Unsplash
Loading...

