Japan Created Lab-Grown Blood That Works for Everyone and Lasts for Years
What if the one thing that could save your life in a crisis—wasn’t available when you needed it most?
Imagine this: a young mother starts hemorrhaging during childbirth in a rural clinic. A car crash victim bleeds out in the back of an ambulance before reaching the hospital. A cancer patient awaits a critical transfusion—but the right blood type isn’t in stock.
Every year, millions of people face this reality. Not because medicine has failed, but because supply has.
Blood—the very essence of life—has an expiration date. It must be matched, refrigerated, and delivered in time. And the world isn’t keeping up. Fewer donors, aging populations, and logistical gaps have created a silent emergency, especially in countries like Japan, where nearly one-third of the population is over 65.
But now, something extraordinary is happening.
In a quiet lab in Nara, Japan, scientists have created blood that defies the rules. It’s lab-grown. It works for everyone. It lasts for years. And yes—it’s purple.
It sounds like science fiction. But it’s very real. And it could change how we think about medicine, emergencies, and even what it means to give life.
Why We Need a Better Blood Supply
We tend to take donated blood for granted—until it’s not there. Behind every unit of blood is a fragile supply chain, built on the generosity of healthy donors and the ticking clock of perishable cells. But what happens when that chain begins to break?
Japan is already living that question. With nearly 30% of its population over the age of 65, the country faces a unique demographic storm. Older adults are not only more likely to require transfusions—they’re less likely to donate. And while guidelines technically allow older individuals to give blood, health conditions and frailty often rule them out. As a result, Japan’s blood donor base is shrinking while demand continues to rise.
BREAKING:
— Current Report (@Currentreport1) June 1, 2025
Japan has developed a universal artificial blood called 'Deoxy-HbV' that remains shelf-stable for up to 2 years—far longer than natural blood, which lasts only a few weeks.
This breakthrough could help address global blood shortages. pic.twitter.com/AbKRvRDEMp
But this isn’t a localized issue. Blood shortages are a global concern. In India, rural clinics frequently lack access to the right blood types. In the U.S., trauma centers operate under pressure to match blood in minutes. Across Africa, blood loss during childbirth remains a leading cause of maternal death—not because the treatments don’t exist, but because the blood simply isn’t there.
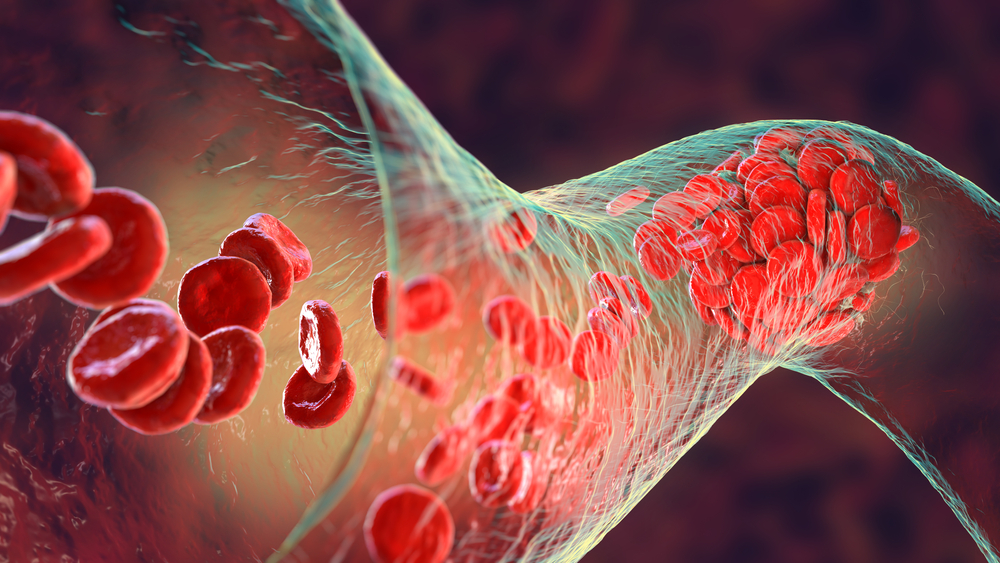
Then there’s the matter of shelf life. Red blood cells stored under ideal refrigerated conditions last about 30 to 42 days. That’s just over a month to collect, process, test, ship, and use them—before they expire. In disaster zones or under-resourced regions, where access and infrastructure are inconsistent, this time limit can turn life-saving medicine into wasted potential.
To make matters worse, compatibility issues slow everything down. Every transfusion must match a patient’s blood type. In an emergency, those few minutes spent verifying blood types can cost lives.
What Makes Japan’s Artificial Blood So Revolutionary

At the center of this breakthrough is a quiet revolution taking place at Nara Medical University. A team led by Professor Hiromi Sakai has developed lab-grown red blood cells that may one day eliminate the most stubborn limitations of blood transfusion. These aren’t ordinary cells—they’re engineered for resilience, universality, and long shelf life.
Let’s break down what makes this innovation so revolutionary:
- Universal Compatibility: Unlike donated blood, which must be matched by blood type, Japan’s artificial blood can be used on any patient, at any time. It sidesteps the ABO system entirely. In an emergency—where minutes matter and blood type isn’t always known—this is a game changer.
- Extended Shelf Life: Regular red blood cells last a little over a month, even under careful refrigeration. These artificial cells? They can be stored for up to two years at room temperature. That changes everything for rural clinics, disaster relief teams, and military medics who work far from high-tech storage facilities.
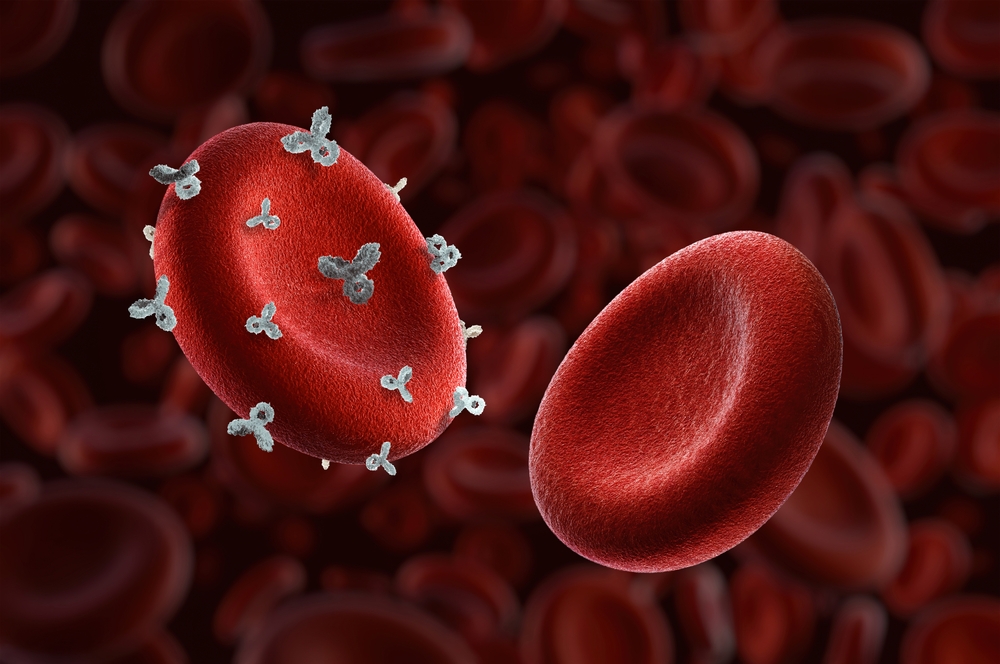
- Safe and Sterile: The artificial blood is made from hemoglobin extracted from expired donor blood that would otherwise be discarded. Researchers then seal this hemoglobin in a virus-proof shell, making it safe from pathogens and contamination. No viruses, no infections—just oxygen-carrying power.
- Purple by Design: Interestingly, the final product isn’t red—it’s purple. That’s due to the unique structure of the synthetic hemoglobin. But function outweighs form: what matters is that it delivers oxygen like real red blood cells—and in early tests, it does.
- Eco-Friendly and Efficient: By repurposing expired blood, the process reduces waste while maximizing medical value. It’s not just innovation—it’s sustainability in action.
This isn’t the only attempt at creating artificial blood, but Japan is closer than most to real-world use. Their upcoming clinical trials mark a critical step: testing the safety and effectiveness of this purple liquid in human volunteers. If all goes well, the country could see practical use by 2030—making Japan the first in the world to implement artificial blood for widespread medical care.
The Science Behind the Discovery

It starts with hemoglobin, the iron-rich molecule inside red blood cells that carries oxygen throughout the body. Hemoglobin is what makes blood so essential in keeping our tissues and organs alive. Japanese researchers, led by Professor Hiromi Sakai of Nara Medical University, found a way to extract this molecule from expired donor blood—the kind that would normally be thrown away once it’s past its safe transfusion date.
Then comes the brilliant part: encapsulation. Scientists take this hemoglobin and encase it in a synthetic, virus-proof shell. This shell protects the hemoglobin, keeps it stable, and mimics the function of a natural red blood cell. The result is a tiny artificial red cell—small enough to circulate through the body’s smallest capillaries, and strong enough to survive in extreme conditions without refrigeration.
Unlike donated blood, these lab-grown cells don’t carry surface antigens, meaning they lack the markers that determine blood type (A, B, AB, or O). That makes them universally compatible—a feature that could eliminate the need for compatibility testing before a transfusion.
Another key player in this field is Professor Teruyuki Komatsu of Chuo University. His team is developing albumin-encased hemoglobin, a synthetic oxygen carrier designed not just to mimic red blood cells, but to also stabilize blood pressure and support critical functions in patients suffering from strokes, hemorrhages, or brain trauma. In animal studies, these carriers have shown promise in keeping organs oxygenated during extreme blood loss.
Some efforts even begin at the cellular level—with hematopoietic stem cells. These special cells, capable of producing all types of blood cells, are being grown in lab environments and gene-edited to boost output and remove blood group markers. Professor Cedric Ghevaert at the University of Cambridge has helped pioneer this method, and while it’s not the path Japan’s current project is using, it represents another promising track in the race toward synthetic blood.
All of this technology—whether stem-cell derived or hemoglobin-based—is pushing medicine toward a future where we no longer rely solely on the fragile, donor-based system we’ve inherited.
The Human Impact
Picture a remote village where a woman goes into labor and starts to hemorrhage. The local clinic has no refrigerator, no matching blood, and no time. Or think of a natural disaster—an earthquake, a flood—where ambulances scramble through rubble, unable to carry enough blood for every victim because of type mismatches and storage limits. Now imagine a world where those obstacles vanish. A packet of universal, room-temperature-stable blood gets pulled off a shelf, administered without delay, and a life is saved—without the usual race against time.
That’s the power of Japan’s artificial blood. It turns every ambulance, every aid truck, every small-town clinic into a fully stocked transfusion center.
This innovation isn’t just poised to impact Japan. Its ripple effect could transform care in developing nations, where blood shortages are often chronic and infrastructure is limited. In India, for example, blood availability continues to fall short of national needs—especially in rural areas. In Africa, postpartum hemorrhage remains a leading cause of maternal mortality. Universal synthetic blood could bridge these deadly gaps.

The human impact extends to war zones, where the ability to treat trauma quickly often determines survival. It could help in stroke care, where Professor Komatsu’s oxygen carriers might prevent brain damage during precious early minutes. It could make risky surgeries safer in under-equipped hospitals. It could reduce the need for large-scale blood donation drives—and lessen dependence on rare blood types, which are often in critically short supply.
And in emergencies, it would do something no traditional blood ever could: eliminate waiting.
As one Reddit user put it, “If this works and isn’t crazy expensive, it will be completely transformational.” That’s not an exaggeration. It’s a sentiment echoed by healthcare workers, disaster responders, and families who have lived through moments where a few milliliters of the right blood could’ve changed everything.
Perhaps the most powerful proof of blood’s impact comes from a man named James Harrison. Known as “The Man with the Golden Arm,” he donated blood every few weeks for over 60 years, helping save an estimated 2.4 million babies with a rare antibody in his plasma. His story is a testament to the extraordinary things one person can do—but also a reminder of how fragile and rare such lifelines can be.
Now imagine if we could multiply that kind of gift. Scale it. Make it global.
Where We Are Now—and What Comes Next
In July 2024, Nara Medical University announced a major step forward: beginning in March 2025, a clinical trial will test the safety of their artificial red blood cells in healthy adult volunteers. Participants will receive between 100 to 400 milliliters of the lab-grown blood. The trial’s first goal is simple but vital: confirm that the synthetic blood causes no side effects when introduced into the human body.
If the initial phase succeeds, researchers will advance to testing efficacy—how well the artificial blood delivers oxygen, integrates with the circulatory system, and performs under real clinical conditions. From there, the timeline stretches toward 2030, when Japan hopes to bring the product into regular hospital use. If successful, it would mark the first time in history that artificial blood is used broadly in real-world medicine.
The implications reach far beyond Japan’s borders. If proven safe and effective, this technology could be adopted globally, particularly in nations facing persistent blood shortages or emergency care bottlenecks. Think India, where maternal mortality remains high. Think sub-Saharan Africa, where rural care lacks critical resources. Think conflict zones, where transporting compatible blood is a logistical impossibility. This is a solution designed not just for hospitals in Tokyo, but for tents in the aftermath of earthquakes, mobile units in refugee camps, and remote clinics in underfunded health systems.
Of course, challenges remain. The artificial blood must pass rigorous safety benchmarks and win approval from global regulatory bodies. Cost, too, will be a factor. While production costs have fallen—from over $90,000 per unit a decade ago to under $5,000 today—they must drop further to rival the $200–$300 range of conventional donated blood. But history shows us that medical costs decline with scale, and the potential here is immense.
Other nations are watching closely. The U.K. has already transfused lab-grown red cells into human volunteers. The U.S. military is investing heavily in synthetic substitutes like ErythroMer, hoping to save lives on the battlefield. Japan may be leading the charge, but the global race is on—and collaboration, not competition, may ultimately drive this technology forward.
The Blood That Unites Us
Strip away the science, the patents, the protocols—and what are we really talking about here?
We’re talking about the most basic element of life: the blood that flows through every human being, regardless of race, religion, or nation. We’re talking about a future where your survival doesn’t depend on finding a match, or being near a fridge, or living in the right part of the world. A future where every person has access to a lifeline, even if that lifeline was created in a lab.
In a world so often divided by borders and identities, this synthetic blood tells a different story—a story of connection. Because if blood is life, then universal blood is unity. It’s the idea that when the worst happens, we don’t need to ask who you are before we help. We just help.
And there’s something deeply poetic about that.
Japan’s creation of artificial blood isn’t just a technological triumph. It’s a reminder of what we’re capable of when we innovate with purpose—when we choose to solve problems not just for profit, but for people. It’s a testament to the belief that every life is worth saving, even when the traditional ways of saving them fall short.
Maybe the color of the blood is purple. Maybe it doesn’t look the way we expect. But in a moment of crisis, color doesn’t matter—function does. And so does compassion.
As we move toward 2030, we stand at the edge of something quietly revolutionary. Not just in medicine, but in mindset. Because what Japan is doing isn’t just building a better blood supply. It’s building a new way of thinking about what’s possible when we refuse to accept limits—when we say no to scarcity and yes to solutions.
So here’s the reflection I’ll leave you with:
In a world where we’re so often asked to divide and define ourselves, what if the future was built on something that works for everyone—no questions asked?
Maybe that future is already pulsing in the purple blood of progress.
Loading...

