Researchers discover brain cell protein that reverses memory decline without removing Alzheimer’s plaques.
Alzheimer’s doesn’t just steal memories—it unravels lives. It takes loved ones from us while they’re still here, replacing familiar smiles with blank stares, shared stories with silence. And for decades, the best our science could offer were temporary lifelines—treatments that eased symptoms but couldn’t touch the deeper truth. The disease kept marching on, and hope began to feel like a myth. We believed we understood the cause. We thought plaques in the brain were the enemy, and clearing them was the path to healing. But what if we were wrong?
In labs from California to Brazil, researchers are uncovering something revolutionary: memory can return—even when plaques remain. Healing may not lie in removing what’s broken, but in restoring what still works. Astrocytes, the brain’s long-overlooked support cells, are stepping into the spotlight. Proteins like hevin, and innovative gene therapies, are pointing us toward a different kind of medicine—one that doesn’t just fight decline, but nurtures regeneration. And with every new discovery, we’re beginning to see Alzheimer’s not as a sentence, but as a challenge we are learning to meet.
Shifting the Focus — Beyond Plaques and Into the Cells
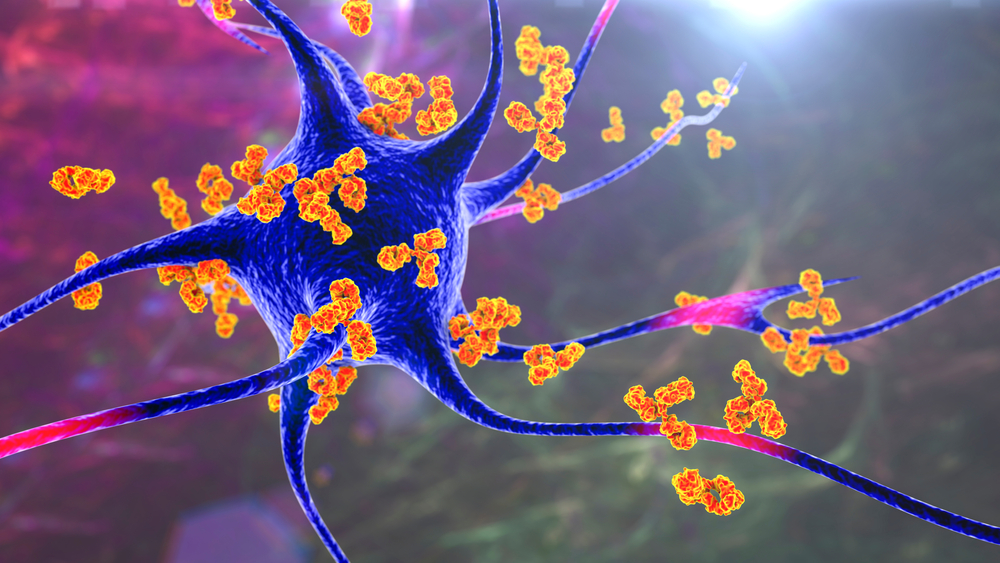
For decades, Alzheimer’s research has been fixated on one primary suspect: beta-amyloid plaques. These protein clumps, which accumulate in the spaces between neurons, have been considered a hallmark of the disease and, for many, its root cause. As a result, most treatments have been developed to target and reduce these plaques, often with limited or temporary results. Even when successful at clearing the plaques, many of these approaches failed to meaningfully improve memory or slow cognitive decline. The persistence of symptoms despite plaque reduction has raised a critical question in the scientific community—what if we’ve been focusing on the wrong enemy?
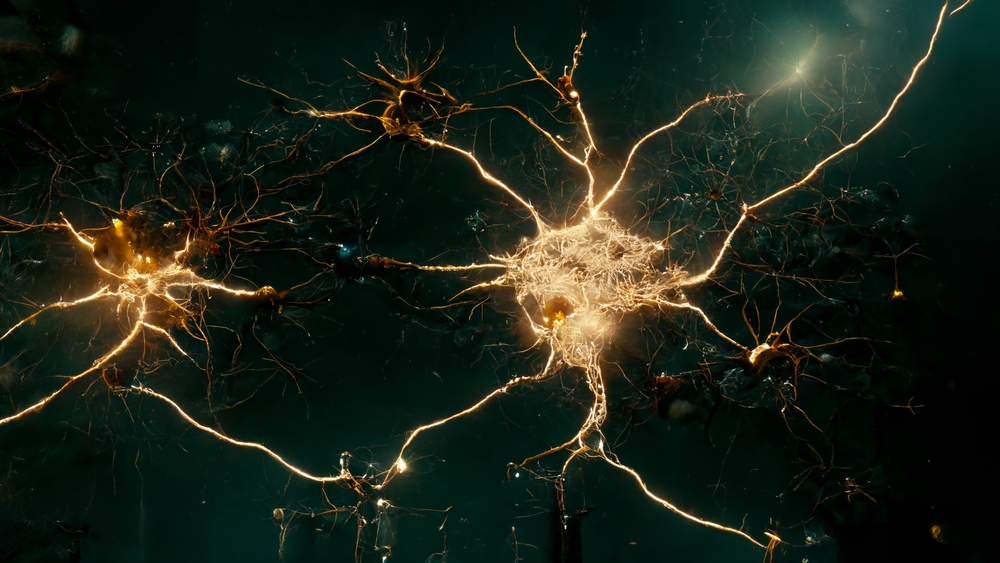
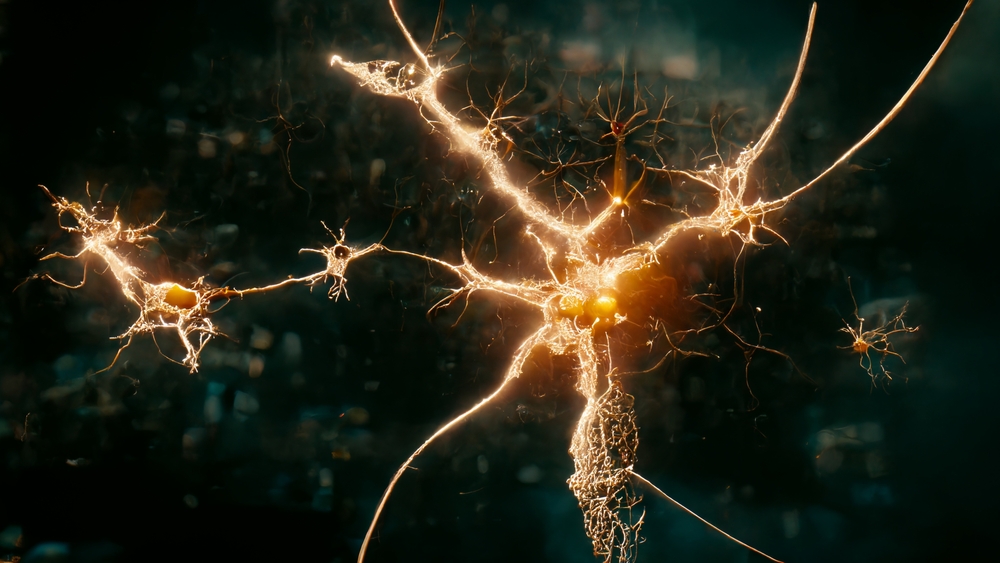
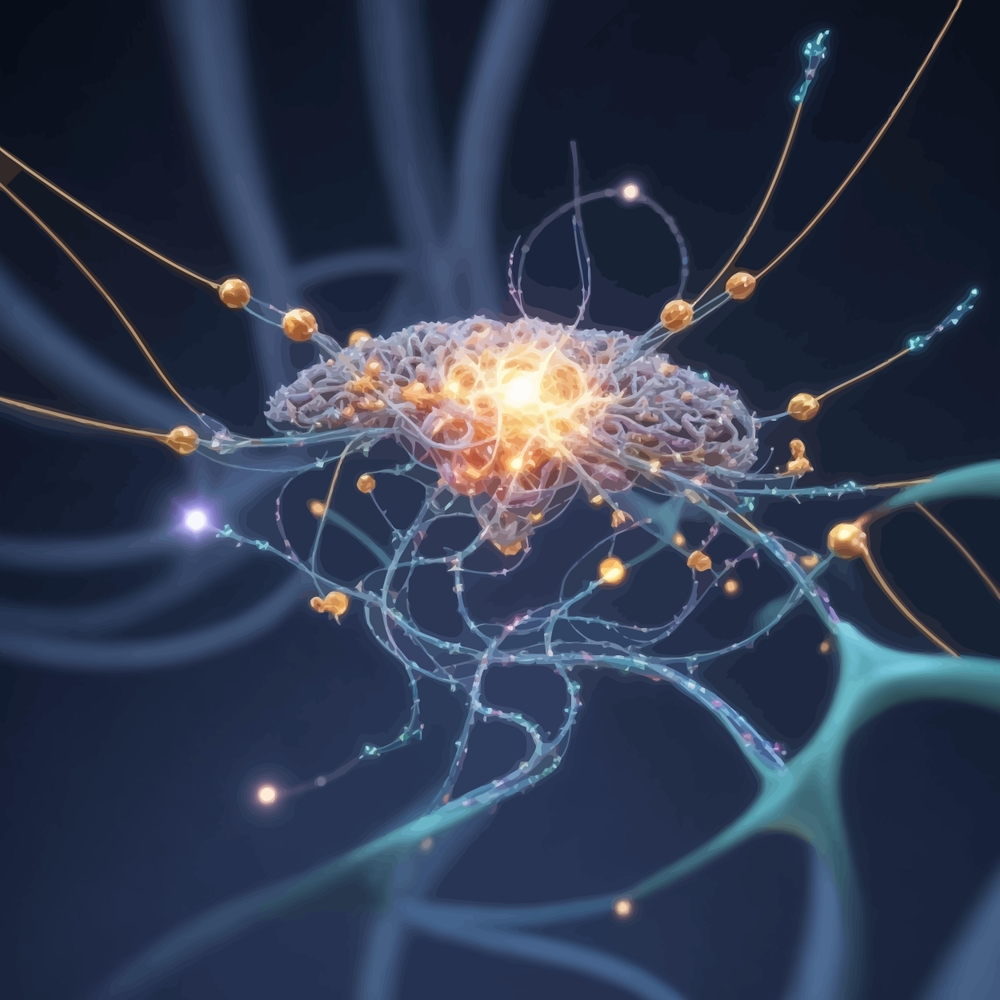
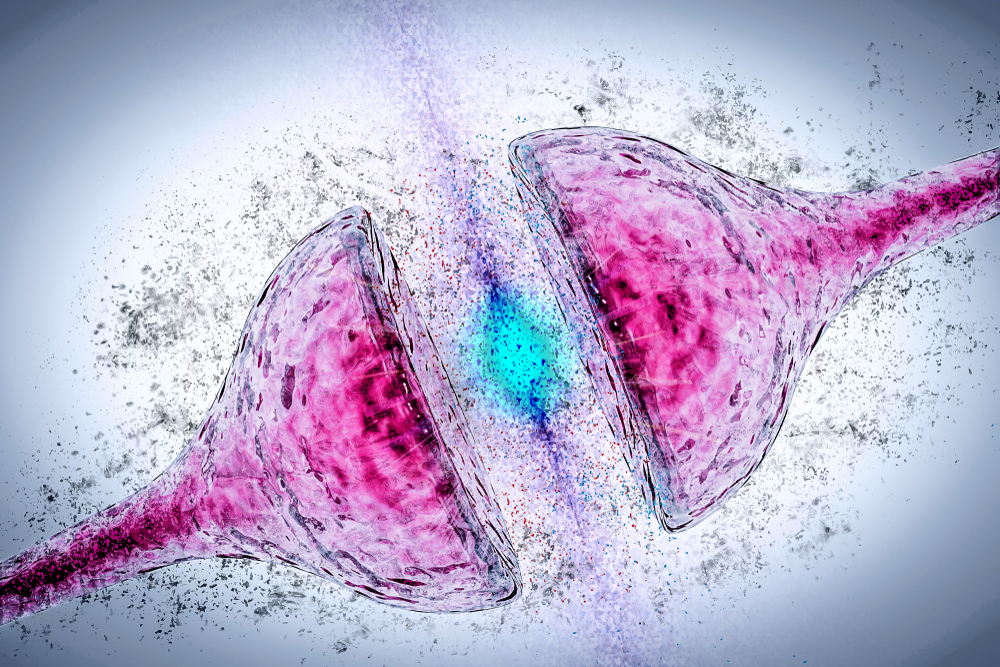
Emerging research is beginning to reshape that conversation. Rather than targeting the plaques directly, scientists are now exploring therapies that influence the behavior of brain cells themselves, particularly a group of supportive cells called astrocytes. These cells don’t carry electrical signals like neurons, but they play a crucial role in maintaining the health of synapses—the communication bridges between neurons. A protein called hevin, produced naturally by astrocytes, has come under the spotlight for its role in supporting synaptic plasticity and cognitive function. In a recent study from Brazil, boosting hevin levels in mice—without altering plaque accumulation—led to significantly improved memory and learning. This protein appears to activate other molecules that support synapse integrity, essentially enhancing the brain’s internal repair mechanisms without engaging the traditional plaque-removal pathway.
The implications of this shift are significant. If cognitive decline can be reversed or prevented by targeting cellular health and synaptic resilience—independent of amyloid plaques—it challenges the long-held belief that plaque buildup is the central cause of Alzheimer’s. This aligns with findings from researchers at the University of California San Diego, who developed a gene therapy that improved memory in symptomatic mice by altering brain cell gene expression, restoring them to a more youthful state. Again, these improvements occurred without reducing the amount of plaque in the brain, suggesting that restoring function might be more critical than removing damage. This evolving understanding opens new avenues for treatment, ones that prioritize cellular rejuvenation and brain network restoration over merely clearing debris.
The Unsung Heroes of the Brain — Astrocytes and the Power of Hevin
While neurons often take center stage in discussions about brain health, it’s the lesser-known astrocytes that are now being recognized as critical players in cognitive resilience. Long viewed as passive support cells, astrocytes are proving to be far more active in regulating brain function than previously understood. They help maintain the environment around neurons, clear out waste, and most importantly, foster the health and strength of synapses. These are the very connections that allow memory, learning, and thought to occur—and their deterioration is a hallmark of Alzheimer’s disease. Scientists are beginning to understand that when astrocytes falter, synapses weaken and brain function declines, regardless of the presence of plaques.
At the heart of this new insight is hevin, a protein secreted by astrocytes that plays a key role in synaptic development and plasticity. In the recent Brazilian study, increasing hevin levels in the brains of aging and Alzheimer’s-like mice triggered a cascade of molecular activity that revitalized neuron communication. Treated mice showed marked improvements in learning and memory tasks, as well as enhanced synaptic connectivity seen on brain scans. Interestingly, this cognitive recovery occurred without any reduction in amyloid plaques, reinforcing the idea that synaptic dysfunction—not plaque presence alone—may be the real driver of memory loss. The researchers also found that Alzheimer’s patients had abnormally low levels of hevin in their brains, suggesting a potential biomarker and therapeutic target for future interventions.
This discovery shifts the spotlight from the traditional “neurons first” model to a broader, more integrated view of brain health. It suggests that effective Alzheimer’s treatment may lie not in attacking the byproducts of a broken system, but in empowering the very cells that maintain that system. By restoring the brain’s internal caretakers—the astrocytes—and boosting molecules like hevin that reinforce communication between neurons, we may be able to halt or even reverse the disease process at its roots. It’s a radical reimagining of how we treat neurodegeneration: not just by cleaning up damage, but by strengthening the architecture that prevents damage in the first place.
Gene Therapy as Restoration, Not Just Defense
In parallel to the work on hevin, scientists at the University of California San Diego are pioneering a gene therapy that also takes a restorative approach—but with a different mechanism. Instead of introducing a specific protein, this therapy rewires the behavior of brain cells at the genetic level. Delivered at the symptomatic stage of Alzheimer’s in mice, the treatment helped preserve memory tied to the hippocampus—the brain’s memory center—and reshaped gene expression in affected brain cells to resemble that of healthy ones. This shift suggests a reversal of disease-driven cellular behavior, not merely a slowing of decline. The promise here lies not in halting the spread of damage, but in restoring functionality to cells that were already compromised.
What sets this approach apart from traditional therapies is that it doesn’t attempt to eliminate the visible signs of Alzheimer’s—like amyloid plaques—but instead focuses on correcting the internal dysfunction within cells. The treated mice demonstrated preserved cognitive function even in the presence of those same toxic plaques, reinforcing the emerging perspective that these proteins may be symptoms rather than causes of the disease. This insight echoes the findings from the hevin research and further supports a growing hypothesis: that cellular health and communication, not just plaque levels, are the most critical predictors of cognitive decline.
Notably, the UC San Diego gene therapy has already taken its first steps toward potential clinical use. Licensed to Eikonoklastes Therapeutics, the technology has received Orphan Drug Designation from the FDA for application in ALS—a separate but related neurodegenerative condition—underscoring its broader relevance in brain health. While much work remains before it can be applied to human Alzheimer’s patients, these developments point to a future where we don’t just manage symptoms but actively restore the biological harmony that enables memory, learning, and thought. It’s a therapeutic vision rooted in regeneration rather than resistance—a shift from fighting disease to rebuilding the systems it disrupts.
Rethinking the Cause — Is It Time to Move Past the Plaque?
For years, the presence of beta-amyloid plaques has been treated as both a diagnostic marker and a primary cause of Alzheimer’s disease. But the more we learn, the more this assumption appears oversimplified. In both the hevin study and the gene therapy research, cognitive improvement occurred without any reduction in plaque buildup. These findings add weight to a growing body of evidence suggesting that plaques may not be the root of the disease, but rather a byproduct—or even a distraction from what truly drives neurodegeneration. As scientists like Felipe Cabral-Miranda have noted, plaques may be involved in the progression of the disease but are not enough on their own to cause it. In other words, we may have been focusing on the smoke while ignoring the fire.
This reframing forces us to look deeper into the mechanics of brain aging. Rather than zeroing in on the visible damage, researchers are beginning to explore the subtle breakdowns in cellular relationships, communication networks, and molecular balance that happen long before symptoms appear. Astrocytes, synaptic integrity, and the proteins that govern neural plasticity are now being recognized as key players—possibly more central than the plaques themselves. This doesn’t mean plaques are irrelevant, but it does challenge the idea that clearing them is the definitive path to a cure. The brain, it turns out, is more than the sum of its pathologies; it’s a dynamic system that, when given the right tools and support, may be capable of healing from within.
This evolution in thinking isn’t just scientific—it’s philosophical. It urges us to stop treating symptoms in isolation and start restoring systems as a whole. That means developing therapies that don’t just aim to remove what’s wrong but nurture what’s right. It means listening to the cells we once overlooked—like astrocytes—and recognizing their potential as healers. And it means being willing to let go of outdated theories in favor of what the evidence now tells us: that true progress will come not from fighting the disease as we’ve known it, but from understanding the brain in all its complexity, and treating it with the nuance it deserves.
From Breakdown to Breakthrough — A New Story for the Mind
What if we’ve been telling ourselves the wrong story about Alzheimer’s—not just in science, but in how we think about the brain, aging, and decline? For too long, we’ve viewed the mind as something that inevitably deteriorates, as though memory is a sandcastle and time the rising tide. But these new discoveries challenge that fatalism. They remind us that the brain is not just vulnerable—it is adaptable, regenerative, and far more resilient than we give it credit for. Healing, it turns out, may not come from attacking what’s broken, but from reigniting what still works within.
The message here is bigger than medicine. It’s about hope backed by science. It’s about a shift from managing decline to enabling recovery—one that mirrors the deeper truth that growth is always possible, even in places that seem lost. The brain, like the human spirit, responds to nurturing. And when we stop seeing age or disease as an ending, we start creating space for restoration, reinvention, and renewal.
This is a call not just to researchers and doctors, but to all of us. To rethink how we care for our minds, how we talk about aging, and how we support those living with Alzheimer’s—not with despair, but with belief in what might still be possible. Because in the end, the most powerful breakthroughs don’t just change science—they change perspective. They whisper, “There is still more to understand. There is still more to heal.”
Loading...

