The Bacteria In Your Gut May Cause Depression, Not The Brain, Claims New Study
What if I told you that your sadness, your low energy, that heavy fog you can’t shake—what if it wasn’t just in your mind? What if part of your struggle came from something invisible, living inside you, reacting to the world you didn’t even realize you were consuming? We’re told to look inward when we feel broken. To “think positive,” to “shift our mindset.” And yes, the mind is powerful. But sometimes, the root of our suffering isn’t in our thoughts—it’s in our biology. In our immune system. In our gut.
A groundbreaking study has revealed something wild, something sobering: a common gut bacterium, exposed to everyday chemicals found in our personal care products, can spark an immune reaction that may trigger depression. Not in metaphor. Not in theory. But through a clear biochemical pathway, one molecule setting off another, like a row of dominos falling silently beneath the surface. This changes the game. Because it means some people’s pain might not come from a lack of willpower or mental discipline—but from a microscopic war happening inside them.
The Mirror in Your Gut—What This Means for You and Us
What if the battle some people are fighting in their minds is actually starting in their bodies—and the trigger is something they never chose? A chemical in their shampoo. A bacterium in their gut. An invisible fire in their immune system. This discovery doesn’t just challenge how we understand depression—it challenges how we understand ourselves. It reminds us that we are ecosystems, not machines. That our moods and mental health are not isolated events but the echo of countless interactions—between body and environment, bacteria and chemistry, mind and immune system. It’s not weakness. It’s biology. It’s reality.
And yet, within this complexity is power. Because the same science that reveals the problem also points to a path forward. We can demand cleaner products and stronger regulations on chemicals like DEA. We can begin to treat inflammation, not just emotion. We can support research that looks beyond symptoms and into root causes. But perhaps most importantly, we can stop judging ourselves or others for struggles that may have origins far beyond what we can see or control. Depression isn’t always just in your head. Sometimes it’s in your gut, your blood, your cells—asking for help
So the next time you look in the mirror, remember: your story is written not just in thoughts and memories, but in molecules and microbes. And if something as small as a bacterial lipid can change the course of a person’s mental state, then perhaps it’s time we shift the way we think about healing—from the inside out, with more compassion, more science, and more courage. Your health is not separate from the world around you—it’s shaped by it. And the more we understand that truth, the closer we get to a future where no one’s suffering is ignored, mislabeled, or misunderstood.

A New Player in Depression—Hiding in Your Gut
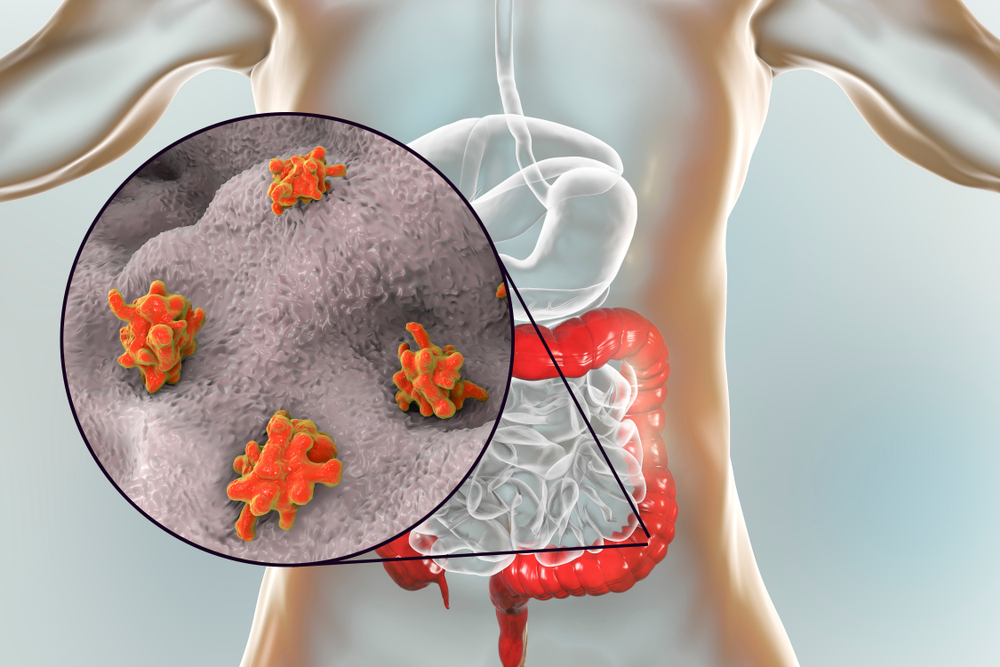
For decades, we’ve been told that depression is a brain problem—a chemical imbalance in the head. But what if the root of some people’s suffering is deeper, quieter, and far more unexpected? A new study out of Harvard Medical School and the Broad Institute suggests that a common gut bacterium, Morganella morganii, might play a direct role in triggering depression. And not through some vague microbiome-gut connection—we’re talking about a precise, molecular-level mechanism involving environmental chemicals, inflammation, and immune activation.
Here’s how it works: M. morganii comes into contact with a widely used chemical called diethanolamine (DEA), found in many industrial and personal care products. This chemical isn’t just passing through—it’s being absorbed and built into the bacteria’s fatty molecules, creating a modified lipid unlike anything seen before. These lipids, now laced with DEA, don’t sit quietly in the gut. They activate powerful immune sensors in the body—specifically TLR1 and TLR2—which then trigger the release of interleukin-6 (IL-6), a signaling protein heavily linked to inflammation. And here’s the critical piece: elevated IL-6 levels have been consistently associated with major depressive disorder. What the researchers found was not just correlation but a direct immune response provoked by a bacterial interaction with a man-made pollutant, adding a whole new layer to how we understand the origins of depression.
This mechanism isn’t speculative. It’s biochemical. It reveals that depression—at least for some individuals—may not originate solely from brain chemistry or trauma, but from a biological cascade that begins in the gut, fueled by environmental contaminants most of us are exposed to every day. That means a bacterial lipid altered by a chemical in your soap or shampoo could end up flipping your immune system into high alert, quietly setting the stage for long-term mental health consequences. The modified lipids created by M. morganii (named MmDEACLs) aren’t just random noise—they’re inflammatory messengers capable of impacting mood, brain function, and emotional resilience through the immune system. As lead researcher Dr. Jon Clardy said, DEA’s transformation into an immune signal was “completely unexpected”—but now, impossible to ignore.

When the Immune System Talks, the Brain Listens
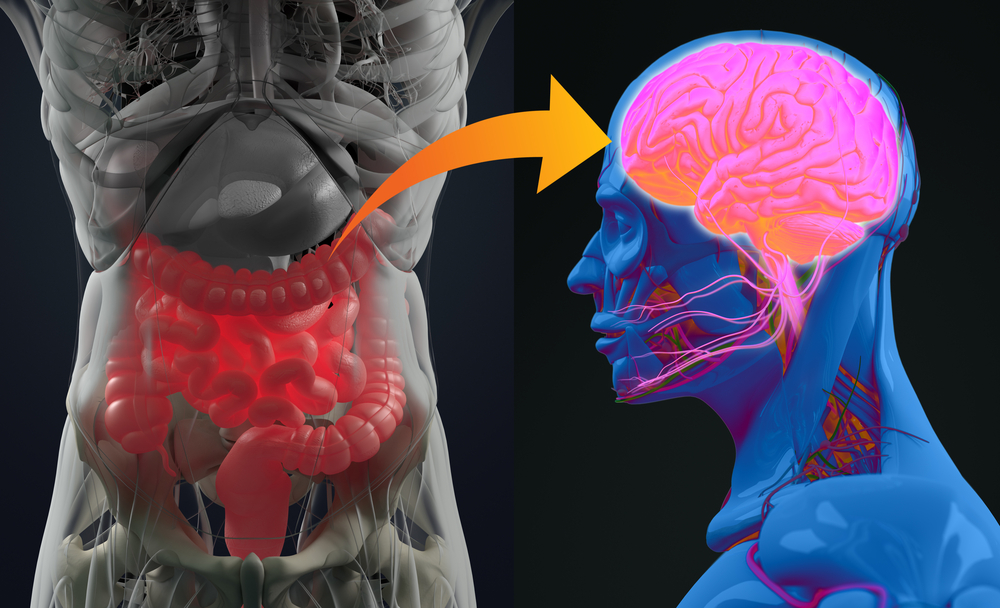
Inflammation isn’t just about swelling or fever—it’s a biological alarm system. And when that system stays activated for too long, it can start rewiring the brain. That’s where interleukin-6 (IL-6), the inflammatory molecule released in response to DEA-modified bacterial lipids, becomes crucial. Chronic exposure to IL-6 has been repeatedly linked to major depressive disorder in both genetic and biochemical studies. Elevated levels of this molecule don’t just stay in the bloodstream—they influence brain regions responsible for mood, decision-making, and emotional regulation, especially the hippocampus and prefrontal cortex.
Research has shown that IL-6 can disrupt the balance of neurotransmitters like serotonin and dopamine, interfere with neuroplasticity, and even reduce the brain’s ability to form new neurons. Over time, this inflammatory state can impair communication between brain cells, slow down cognitive functions, and increase vulnerability to stress—all of which are hallmarks of depression. In this sense, the immune system isn’t just a bystander in mental health—it’s an active participant, shaping how we feel, think, and respond to life’s challenges. And when it’s chronically activated by signals coming from the gut, it creates a feedback loop: inflammation fuels depressive symptoms, which can, in turn, worsen gut health and immune dysfunction.
This connection transforms how we think about mental illness. It suggests that for some individuals, depression may not be just a psychological or emotional struggle—it may also be a form of neuroinflammation. And if that’s the case, then the solutions we need might look different too. Instead of targeting only neurotransmitters with medication, we might also need to calm the immune system, restore gut health, and reduce environmental exposures that quietly set this chain reaction in motion. The brain and body are in constant conversation, and inflammation is one of the loudest voices in the room.

Pollution in the Mirror—The Everyday Chemicals We Absorb
We often think of pollution as something “out there”—smog in the sky, oil in the ocean, plastic in the streets. But what happens when the pollution is inside us? Diethanolamine (DEA), the chemical at the center of this gut-brain discovery, isn’t some exotic industrial hazard. It’s found in everyday items like shampoos, soaps, cosmetics, and cleaning products. For most people in developed countries, exposure is routine and nearly unavoidable. That means the raw material for this inflammatory cascade is already present in millions of bodies, quietly circulating and interacting with the microbial communities inside us.
When Morganella morganii or similar bacteria pick up DEA, they don’t just digest it—they repurpose it. This transformation into immune-activating lipids shows how environmental chemicals, once inside the body, can be woven into biology in unexpected and disruptive ways. It also reveals a hidden vulnerability in the relationship between modern life and mental health. We’ve long known that pollutants can affect hormones and organs, but this research adds a new layer: some pollutants may be influencing how we feel—our moods, our energy, even our sense of self—by altering the behavior of microbes within us. It’s not the kind of effect you notice immediately. It builds slowly, quietly, over time, like rust spreading inside the gears of a machine.
This isn’t just about one chemical or one bacterium—it’s a public health signal. If substances like DEA can be metabolized into pro-inflammatory molecules, there are likely others. And if gut microbes can weaponize these compounds against the immune system, it means our daily chemical exposure isn’t just a toxicology issue—it’s a mental health one too. The implications are vast. It raises questions about how we regulate ingredients in personal care products, what we consider “safe,” and how much we really understand about the long-term effects of living in a chemically saturated world. This isn’t fearmongering—it’s a wake-up call rooted in molecular science.

Rethinking Treatment—Could the Gut Be the New Frontier for Mental Health?
If depression in some cases begins in the gut, then treating it solely in the brain may be like patching a leak without turning off the tap. This discovery doesn’t just open a new window into the biology of depression—it opens an entirely new door for treatment. Current therapies often focus on altering brain chemistry, using antidepressants to boost neurotransmitters like serotonin or dopamine. And while these medications help many, they don’t work for everyone. For those whose depression may be driven by chronic inflammation from gut-derived immune signals, a different approach might be needed—one that targets the source, not just the symptoms.
Imagine a treatment that identifies and neutralizes the specific immune response triggered by DEA-modified bacterial lipids. Or probiotics engineered to crowd out or disable bacteria like M. morganii that turn environmental pollutants into inflammatory triggers. Even more, imagine screening for these modified lipids in blood or stool samples to identify patients whose depression may be inflammation-driven—opening the door to more personalized, biologically informed interventions. Researchers are already asking these questions. While it’s early, the hope is that this kind of precision medicine could offer new paths for people whose symptoms haven’t responded to traditional antidepressants.
This isn’t about replacing psychology or dismissing the emotional realities of depression. It’s about expanding the map. Mental health has always been multifaceted—emotional, psychological, social, and biological. This discovery sharpens the biological side of that picture, showing that microbes and immune signals can be just as influential as thoughts or traumas. Treating inflammation, calming the immune system, or even modifying the gut microbiome could soon be part of the same toolkit as therapy and medication. In the future, healing the mind may also require healing the gut.
The Mirror in Your Gut—What This Means for You and Us
What if the battle some people are fighting in their minds is actually starting in their bodies—and the trigger is something they never chose? A chemical in their shampoo. A bacterium in their gut. An invisible fire in their immune system. This discovery doesn’t just challenge how we understand depression—it challenges how we understand ourselves. It reminds us that we are ecosystems, not machines. That our moods and mental health are not isolated events but the echo of countless interactions—between body and environment, bacteria and chemistry, mind and immune system. It’s not weakness. It’s biology. It’s reality.
And yet, within this complexity is power. Because the same science that reveals the problem also points to a path forward. We can demand cleaner products and stronger regulations on chemicals like DEA. We can begin to treat inflammation, not just emotion. We can support research that looks beyond symptoms and into root causes. But perhaps most importantly, we can stop judging ourselves or others for struggles that may have origins far beyond what we can see or control. Depression isn’t always just in your head. Sometimes it’s in your gut, your blood, your cells—asking for help in a language we’re only now beginning to translate.
So the next time you look in the mirror, remember: your story is written not just in thoughts and memories, but in molecules and microbes. And if something as small as a bacterial lipid can change the course of a person’s mental state, then perhaps it’s time we shift the way we think about healing—from the inside out, with more compassion, more science, and more courage. Your health is not separate from the world around you—it’s shaped by it. And the more we understand that truth, the closer we get to a future where no one’s suffering is ignored, mislabeled, or misunderstood.
Loading...

