A Wearable Kidney May Finally Free Patients From Hospital Dialysis and Restore Real Independence

Imagine if every other day of your life was scheduled around a machine. Three times a week, four hours at a stretch, you sit tethered to tubes while your blood is cleaned. Vacations, family dinners, even the simple joy of drinking a full glass of water must be negotiated with the strict rhythm of this machine. For hundreds of thousands of people living with kidney failure, this is not imagination it is reality.
Dialysis has kept people alive for decades, but it comes with a hidden price. Kidneys are meant to work continuously, 24 hours a day, 7 days a week. Dialysis, by contrast, works in jolts brief, exhausting sessions that leave patients drained, restricted, and perpetually waiting for the next round. Between treatments, toxins build up, energy plummets, and life becomes survival on someone else’s schedule.
Here’s a sobering truth: kidney disease kills more people each year than breast cancer or prostate cancer, and nearly 37 million Americans live with some form of it. Yet the system designed to treat kidney failure is stretched thin. Donor organs are scarce, waitlists stretch for years, and dialysis costs the U.S. government over $100 billion annually. For patients, the cost is even higher: independence, dignity, and time.
But what if the machine could shrink? What if instead of hours in a clinic, treatment slipped quietly into the background something you could wear, or even carry inside your body, while you live, work, travel, and dream again? Scientists are closer than ever to making that future real, and the promise of a wearable or implantable kidney could mark one of the greatest medical breakthroughs of our time.
The Weight of Life on Dialysis
For people whose kidneys have failed, dialysis is more than a treatment it becomes a way of life. In the United States alone, over half a million people depend on it to survive. Most undergo hemodialysis, where blood is filtered through a machine at a clinic three times a week. Each session lasts about four hours, and when you add travel time, recovery, and the toll it takes on the body, entire days are swallowed up. What should be a tool for living often feels like a full-time job with no days off.
The problem is that dialysis is a stopgap, not a substitute. Healthy kidneys never rest; they quietly balance electrolytes, regulate blood pressure, and remove waste every second of every day. Dialysis, by contrast, only works intermittently. That means toxins and fluids build up between sessions, leaving patients feeling sick, weak, or disoriented. Nausea, dizziness, and painful cramps are common side effects. Even when the treatment ends, many patients leave clinics feeling wrung out rather than restored.

Then there are the rules. Because dialysis can’t keep up with the body’s natural rhythms, patients must tightly restrict what they eat and drink. A slice of pizza, an extra glass of water, or too much potassium-rich fruit can become dangerous. These limits often feel like another layer of punishment especially when added to the exhaustion and dependency dialysis creates.
The impact reaches far beyond the body. Studies show higher rates of depression, social isolation, and unemployment among dialysis patients. Planning life around treatment schedules makes it difficult to work full-time, care for family, or simply enjoy everyday moments. Even peritoneal dialysis, which patients can do at home, usually loses effectiveness within a few years, forcing many back into clinics.
Globally, the burden is even heavier. Around 3 million people rely on dialysis, and that number is growing as diabetes and hypertension rise. Yet access is deeply unequal: in wealthier nations, patients are at least guaranteed treatment, though at enormous financial and emotional cost; in poorer regions, dialysis may be unaffordable or unavailable altogether. The U.S. government alone spends more than $100 billion each year on kidney disease care, with dialysis consuming a major share of Medicare’s budget.
Why Innovation Can’t Wait

The numbers tell the story. In the United States, more than 100,000 people are waiting for a kidney transplant at any given time, but only about 20,000 transplants are performed each year. The median wait is 3.6 years, and many patients die before their turn comes. Even for those fortunate enough to receive a new kidney, the battle isn’t over. Transplant recipients must take immunosuppressant drugs for life, trading one set of limitations for another higher risks of infection, diabetes, heart disease, and even certain cancers.
This bottleneck forces the vast majority of kidney failure patients to remain on dialysis indefinitely. The difference between dialysis and natural kidney function is stark. A healthy pair of kidneys filters blood 168 hours a week, nonstop. Dialysis, as it’s commonly provided in the U.S., filters blood for just 12 hours a week. That gap is not just inconvenient; it’s dangerous. It leaves patients vulnerable to complications like cardiovascular disease, metabolic imbalances, and shortened lifespans.
The scale of the problem is staggering. Nearly 37 million Americans have chronic kidney disease, and millions worldwide depend on dialysis. The condition kills more people each year than breast cancer or prostate cancer, yet it receives far less public attention. The financial strain is immense as well: U.S. government spending on kidney disease exceeded $100 billion in a single year, with dialysis consuming a major portion of Medicare’s budget. And those costs will only grow as diabetes, hypertension, and aging populations drive up rates of kidney failure.
The Science Behind Artificial and Wearable Kidneys

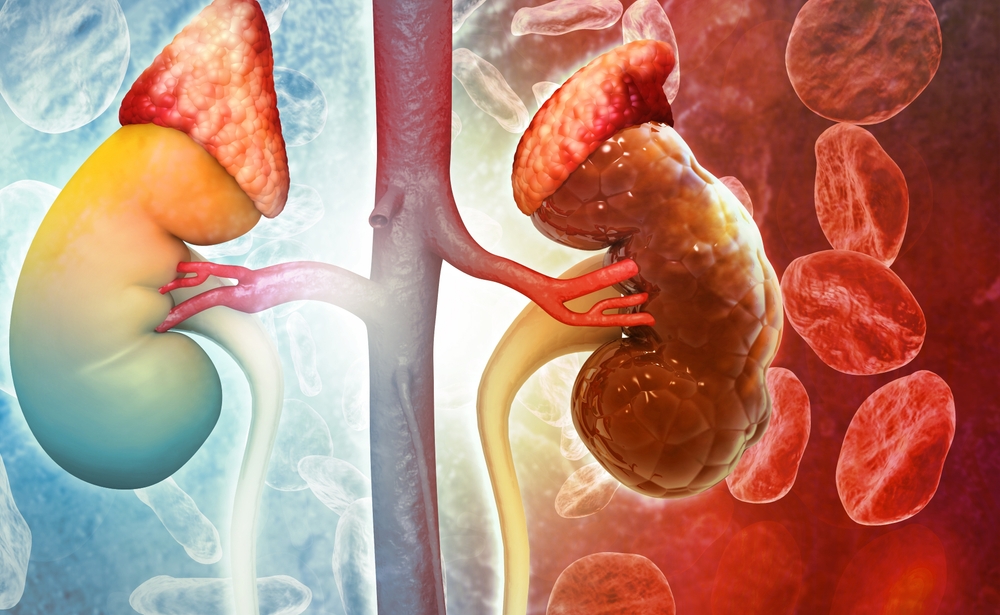
Designing an artificial kidney is one of the most complex challenges in medicine. Unlike an artificial heart, which focuses on pumping blood, or an insulin pump, which regulates a single hormone, the kidneys perform dozens of interconnected tasks simultaneously. They filter waste, balance electrolytes like sodium and potassium, control blood pressure, maintain water balance, and even release hormones that stimulate red blood cell production. To replicate this orchestration in a device is like trying to compress an entire symphony into a single instrument.
Researchers are pursuing two major paths. The first is fully mechanical, using advanced filters and modules to mimic the kidney’s intricate processes. Dr. Victor Kurtz and his team, for example, have developed a man-made system that relies on ultrafiltration, nanofiltration, electrodeionization, and reverse osmosis modules. These components work together to selectively remove toxins, balance salts, and return clean, regulated blood to the body. The device even includes software-driven feedback controls, allowing it to adjust in real time to a patient’s diet or fluid intake.
The second approach combines engineering with biology. The Kidney Project, a collaboration between UC San Francisco and Vanderbilt University, is developing a “bioartificial” kidney that uses living human kidney cells. This device has two parts: a high-efficiency filter to separate waste from the blood and a bioreactor filled with kidney cells to perform delicate regulatory functions. To protect those cells from immune attack, the system uses silicon membranes thinner than a strand of hair, which allow nutrients and oxygen through but block immune cells. This means the device could operate without the lifelong immunosuppressant drugs required after a traditional transplant.
One of the toughest challenges is handling urea, the body’s main nitrogen waste product. Healthy kidneys eliminate large amounts daily, but artificial devices must find efficient, safe, and compact ways to do the same. Teams are experimenting with enzyme-based systems that break down urea, electrochemical methods that convert it into harmless gases, and sorbents that trap it. Each method has pros and pitfalls enzymes can create toxic byproducts, electrochemical systems must avoid generating harmful compounds, and sorbents often struggle with efficiency.
Miniaturization is another frontier. Traditional dialysis machines are massive because they require large volumes of water and dialysate fluid. Wearable and implantable designs must shrink these processes down to a fraction of the size while keeping them reliable and safe. Advances in nanotechnology, membrane chemistry, and battery design are bringing that vision closer to reality.
Recent Breakthroughs and Pilot Studies

One of the most celebrated efforts comes from Dr. Victor Kurtz and his team, who developed a fully man-made artificial kidney. Their project earned the prestigious KidneyX prize a joint initiative of the U.S. Department of Health and Human Services and the American Society of Nephrology recognizing bold innovation in kidney care. The device, which uses advanced filters and electrodeionization modules instead of living cells, has been hailed as one of General Electric’s “Five Coolest Things on Earth.” Dr. Kurtz envisions its evolution in phases: from a desktop device, to a belt-worn portable version, and ultimately to a fully implantable artificial kidney. Early prototypes have already demonstrated superior filtration chemistry and reduced clotting compared to traditional systems.
Meanwhile, the Kidney Project at UC San Francisco and Vanderbilt University has taken a different path, building a bioartificial kidney that integrates living human cells into a silicon-protected bioreactor. In a landmark study, the device functioned inside pigs for a week, performing kidney-like tasks without triggering immune rejection. This milestone is critical, as it suggests such a device could operate in humans without the need for lifelong immunosuppressants a major obstacle to transplantation today.
Wearable dialysis devices have also reached patients in small but significant pilot studies. In 2016, researchers tested a “wearable artificial kidney” weighing about five kilograms. Patients wore it around the waist, powered by standard batteries, while walking freely even leaving the hospital to visit a nearby park. The device provided continuous filtration for hours at a time, and though early prototypes faced challenges with clotting and dialysate regeneration, they proved the concept was workable.
Other innovations are pushing the boundaries of peritoneal dialysis. AWAK Pte Ltd, for instance, has developed a portable device that recycles dialysate fluid, drastically reducing the amount needed. Clinical trials showed it could achieve meaningful reductions in toxins like urea and creatinine while patients went about daily life. In Italy, the ViWAK system has explored wearable peritoneal dialysis with promising results, using sorbent cartridges and compact pumps to maintain round-the-clock clearance.
What a Wearable or Implantable Kidney Could Mean for Patients
For patients, the promise of a wearable or implantable kidney isn’t just medical it’s deeply personal. It’s the possibility of reclaiming something dialysis has long taken away: independence. Instead of shaping every week around clinic visits, treatment could happen quietly in the background, allowing people to work, travel, and live without the constant reminder of their illness.
The health benefits would be equally transformative. Because wearable and implantable devices can operate continuously, they more closely mirror the 24/7 function of natural kidneys. That means fewer dangerous swings in fluid and toxin levels, less cardiovascular strain, and better blood pressure control. Patients might no longer need to restrict every sip of water or calculate the potassium in each meal. For many, it could be the first time in years that eating and drinking feel normal again.
Continuous therapy also reduces complications tied to intermittent dialysis. Studies already show that patients receiving more frequent or longer treatments experience fewer hospitalizations, improved nutrition, and a stronger quality of life. A device that delivers this around the clock would push those benefits even further, lowering the risks of heart attack, stroke, and anemia that plague dialysis patients today.
The ripple effects extend beyond the individual. Families caring for someone on dialysis often face financial stress, lost work hours, and emotional strain. A wearable kidney could ease those burdens by allowing patients to manage their treatment more independently. At a societal level, shifting away from in-center dialysis could save billions in healthcare costs each year. In the U.S., Medicare spends more than $100 billion annually on kidney disease, with dialysis eating up a major share. A portable or implantable solution could free both patients and health systems from these crushing costs.
Even the environment stands to benefit. Traditional dialysis consumes enormous amounts of water and generates tons of disposable plastic waste. Wearable and implantable devices, which use far less fluid and rely on recyclable sorbents or closed-loop systems, could drastically cut the carbon footprint of kidney care.
Ultimately, these technologies represent more than a clever engineering fix. They offer a chance to restore dignity to let people with kidney failure live lives defined not by hospital schedules and fluid restrictions, but by choice, mobility, and connection.
Restoring Freedom, One Kidney at a Time
For decades, dialysis has been a lifeline, but also a leash. It has sustained millions of people with kidney failure, yet it has confined them to routines that strip away time, energy, and independence. The prospect of a wearable or implantable kidney changes that narrative. It suggests a future where treatment no longer dictates life, but instead quietly supports it just as natural kidneys do.
The breakthroughs we’ve seen so far prove that this is not science fiction. Prototypes have already freed patients to walk outside while receiving dialysis, and bioartificial kidneys have functioned inside animals without rejection. These are not just engineering victories; they are glimpses of a new kind of freedom for people who have long been tethered to machines and schedules.
But progress does not happen in isolation. To move from laboratory prototypes to devices in the hands of patients, we need sustained investment, regulatory support, and public awareness. Kidney disease kills more people each year than some of the cancers that dominate headlines, yet it receives far less attention. Changing that imbalance is part of the work.
The promise of a wearable or implantable kidney is not simply about extending life it is about restoring dignity, mobility, and hope. For patients and families, it is a chance to reclaim ordinary moments: traveling without fear, eating without constant calculation, working without exhaustion. For society, it is an opportunity to relieve healthcare systems of a crushing financial burden while embracing a model of care rooted in independence.
Every great leap in medicine has started with a vision that seemed out of reach whether it was organ transplants, artificial hearts, or gene therapies. The artificial kidney is the next leap. And for millions of people worldwide, its arrival cannot come soon enough.
Loading...

