Scientists Find Plant Virus That Trains Immune System to Fight Cancer.
What if the cure for one of humanity’s greatest enemies was hiding in something as ordinary as a bean field? We spend billions searching for cutting-edge technology, complex drugs, and futuristic machines — yet sometimes, nature has already written the answer in places we’ve overlooked. One such answer comes from an unlikely source: a virus that doesn’t harm people at all, a virus that normally lives inside black-eyed peas.
At first glance, the cowpea mosaic virus (CPMV) seems insignificant, the kind of microbe scientists might study only in agricultural labs. But today, researchers are uncovering evidence that this humble plant virus could hold the power to transform the fight against cancer. Instead of spreading illness, it trains the immune system to wake up, to remember its own strength, and to fight back against tumors that once seemed untouchable.
A Surprising Ally in the Fight Against Cancer
Imagine a virus — not one that spreads disease, but one that carries the potential to heal. That’s the surprising promise of the cowpea mosaic virus (CPMV), a microscopic invader that typically infects black-eyed peas. For decades, it was of little interest to medicine, dismissed as just another plant virus with no direct impact on human health. But researchers at the University of California San Diego, working in collaboration with the National Cancer Institute, have discovered something extraordinary: CPMV has a unique ability to awaken the human immune system and redirect it against one of the most devastating illnesses of our time — cancer. This unexpected ally from the plant kingdom is showing that sometimes, the answers to our greatest challenges can come from the most humble and overlooked sources.
What sets CPMV apart is not only its promise but also its accessibility. Most cancer immunotherapies are prohibitively expensive, relying on complex, high-tech manufacturing processes that drive up costs and make treatments available only to a limited number of patients. In contrast, CPMV can be grown in plants using little more than sunlight, soil, and water. The idea that something so simple could rival — and in some ways surpass — advanced biotechnology is both humbling and inspiring. In preclinical studies, when scientists injected CPMV directly into tumors, they witnessed something remarkable. Not only did the virus help destroy the targeted tumor, but it also primed the immune system to hunt down metastatic cancer in other parts of the body. In other words, this plant virus triggered a systemic response, effectively teaching the body to recognize and fight cancer wherever it appeared.
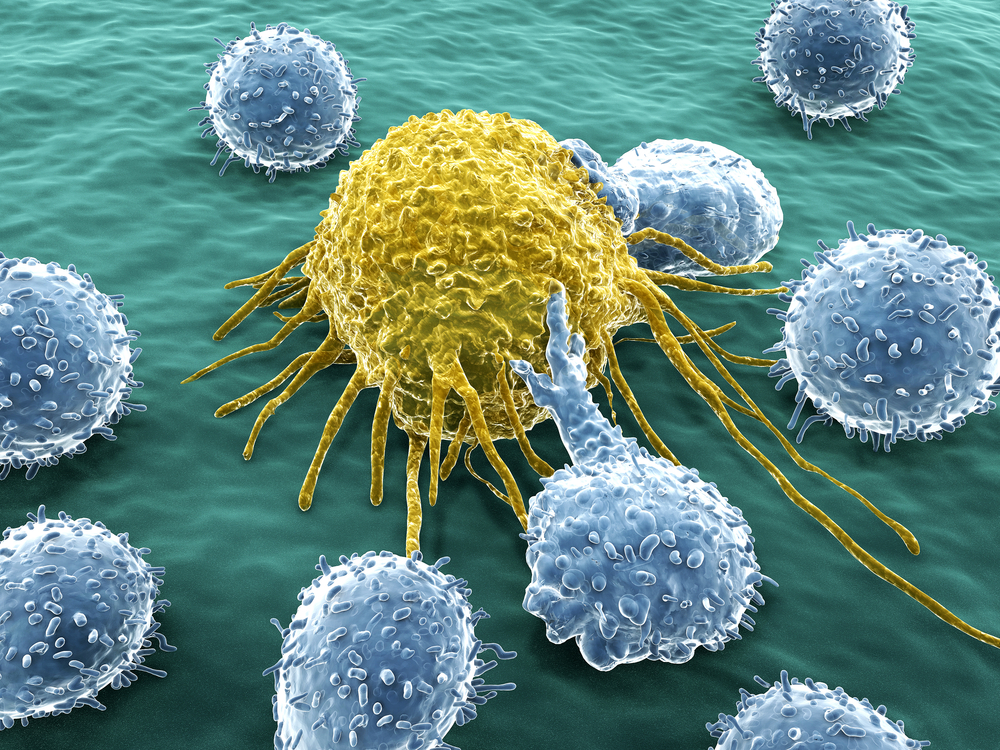
The key lies in the immune system’s reaction. Although CPMV does not infect human cells — it is harmless in that regard — its presence is enough to spark an alarm. The body responds by calling in reinforcements: neutrophils, macrophages, and natural killer cells flood the tumor microenvironment, launching a coordinated attack on the cancer. But the impact does not stop there. CPMV also activates B cells and T cells, the adaptive arm of the immune system, which builds long-lasting memory. This means the body is not only fighting the immediate tumor but is also being reprogrammed to remain vigilant, ready to detect and destroy cancerous cells if they resurface in the future. It is, in essence, an immune awakening — a reminder that within us already exists the machinery to fight disease, sometimes it just needs the right spark to be set in motion.
As Nicole Steinmetz, the lead scientist on the project, observed: “It is fascinating that CPMV but not other plant viruses stimulates an anti-tumor response.” That simple statement carries profound weight. It highlights that nature often holds mysteries we have yet to unravel, and among those mysteries may lie cures to diseases that have plagued humanity for centuries. CPMV represents more than just a scientific breakthrough; it is a window into a future where cancer treatment may become more accessible, more affordable, and more effective. What began as a curiosity in a black-eyed pea field may soon stand at the front lines of medicine’s fight against one of the deadliest diseases of our time.
The Science Behind the Breakthrough
To understand why the cowpea mosaic virus (CPMV) is so effective against cancer, scientists compared it with its close cousin, the cowpea chlorotic mottle virus (CCMV). On the surface, the two viruses look remarkably similar. Both form nanoparticles of comparable size and are absorbed by human immune cells at roughly the same rate. Yet their outcomes could not be more different: CPMV sparks a powerful anti-tumor immune response, while CCMV fails to do so. This puzzle drove researchers to dig deeper, unraveling what makes CPMV unique and why it stands out as such a potent weapon in cancer immunotherapy.
The answer lies in how the human immune system processes these plant viruses once they are inside the body. CPMV stimulates a wide spectrum of interferons — type I, II, and III — which are proteins long known to possess anti-cancer properties. In fact, some of the earliest immunotherapy drugs were based on recombinant interferons, but their use was limited due to side effects and high costs. What CPMV offers is a natural way of activating these same defenses without introducing synthetic compounds. By contrast, CCMV produces a flood of pro-inflammatory interleukins, signaling molecules that stir up inflammation but do little to help the immune system recognize and eliminate cancer cells. This crucial difference explains why CPMV is able to mobilize the immune system so effectively while its cousin falls flat.
Another distinguishing factor is how the viral RNA is processed inside mammalian cells. CPMV’s RNA persists longer and makes its way to the endolysosome, a cellular compartment that activates a protein known as toll-like receptor 7 (TLR7). This receptor plays a pivotal role in detecting viral RNA and jumpstarting antiviral — and in this case, anti-tumor — immune responses. The RNA from CCMV, on the other hand, fails to reach this activation point, rendering it ineffective in turning the immune system against cancer. In essence, CPMV’s architecture and behavior inside immune cells provide it with the keys to unlock a powerful cascade of responses that reprograms the body to see cancer not as a tolerated invader, but as a target for destruction.
By identifying these mechanistic differences, scientists are not only learning why CPMV is effective, but they are also opening the door to refining and improving it for clinical use. Understanding the “why” behind CPMV’s success is a critical step in transforming it from an experimental discovery in the lab to a therapy that could one day be used safely and reliably in hospitals around the world. It reminds us that breakthroughs are rarely accidents; they are the result of persistent curiosity and a willingness to look deeper into what others might have overlooked.
From Lab to Life
While the science behind CPMV is fascinating, the real test lies in how it performs outside the controlled environment of a laboratory. Preclinical studies have already offered promising results. In multiple mouse models, injections of CPMV directly into tumors triggered tumor shrinkage and prevented the spread of cancer to other parts of the body. Even more compelling, trials in canine cancer patients — animals with naturally occurring tumors, not artificially induced ones — showed encouraging signs that this therapy could be effective in larger, more complex organisms. Dogs, who often develop cancers similar to humans, represent an important bridge between lab experiments and human trials, and their positive responses suggest that CPMV has the potential to translate successfully into human medicine.
Equally important is the nature of the immune memory that CPMV creates. Cancer is notorious for its ability to return even after seemingly successful treatment. By activating not only the immediate immune response but also the long-lasting memory of B and T cells, CPMV primes the body to remain vigilant. This means that if cancer cells attempt to resurface months or even years later, the immune system will be better prepared to recognize them and eliminate them before they can grow into new tumors. For patients, this could represent a shift from temporary remission to lasting freedom from the constant fear of recurrence.
Researchers are now working toward advancing CPMV to human clinical trials. This involves rigorous testing to ensure that the therapy is both safe and effective, as well as the painstaking process of identifying the most potent and reliable candidate strains of the virus. Clinical trials are where hope meets reality, and while many experimental therapies fail at this stage, CPMV enters with strong momentum fueled by years of promising data and growing support from institutions like the National Cancer Institute and the American Cancer Society. The path forward may still be long, but the groundwork is being laid for CPMV to one day move beyond experimental treatment and into the realm of real-world medicine.
The transition from lab to life is often the hardest part of scientific discovery. Yet what makes CPMV stand out is that it is not just effective — it is also practical. Its production is relatively inexpensive, requiring only plants and natural resources, making it an attractive candidate for scalable treatments that could reach patients around the world, not just those with access to cutting-edge medical centers. This accessibility gives CPMV the potential to not only save lives but also reduce inequality in cancer treatment, offering hope in places where modern therapies remain out of reach.
Rethinking Immunotherapy
Cancer immunotherapy has long been hailed as one of the most revolutionary advancements in modern medicine. Unlike chemotherapy or radiation, which directly attack tumors but often harm healthy tissue in the process, immunotherapies aim to harness the body’s own defenses to fight the disease from within. Treatments like checkpoint inhibitors and CAR-T cell therapy have changed the landscape of oncology, offering hope where none existed before. Yet these treatments are far from perfect. They can be prohibitively expensive, sometimes costing hundreds of thousands of dollars per patient, and they do not work for everyone. Side effects can also be severe, leaving many patients unable to tolerate the therapy.
What CPMV offers is a new paradigm in immunotherapy. By leveraging a natural virus that cannot infect humans, it sidesteps many of the risks associated with current treatments. Its ability to activate multiple arms of the immune system at once — both innate and adaptive — gives it a versatility that many existing therapies lack. And because it can be grown in plants at low cost, it holds the potential to democratize access to cutting-edge treatment. This combination of effectiveness, safety, and affordability sets CPMV apart as a candidate that could redefine what cancer therapy looks like in the years ahead.
Another striking aspect of CPMV is the way it highlights the overlooked potential of nature. While modern medicine often turns to advanced technology, genetic engineering, or artificial compounds, this discovery reminds us that some of the most powerful solutions may already exist in the natural world, waiting to be uncovered. Plant viruses, which were once seen as irrelevant to human health, are now at the forefront of one of the most pressing medical challenges of our time. This shift in perspective is not just about science; it is about humility — the willingness to learn from the world around us and recognize that wisdom can be found in unexpected places.
As scientists continue to study CPMV, the broader field of immunotherapy may also be transformed. The lessons learned here — about persistence, curiosity, and the importance of investigating the mechanisms behind unexpected phenomena — could inspire new approaches to other diseases. If a virus from a black-eyed pea can teach the immune system to fight cancer, what else in the natural world might hold answers we have yet to imagine?
A Call to Rethink What’s Possible
The story of the cowpea mosaic virus is more than a tale of scientific discovery; it is a reminder of possibility. For patients, it represents a future where cancer treatment may not come at the cost of financial ruin, debilitating side effects, or limited access. For scientists, it is proof that even the most unassuming corners of nature can hold the keys to life-saving breakthroughs. And for all of us, it is an invitation to rethink what is possible when we combine curiosity, perseverance, and an openness to learning from the unexpected.
Too often, we see cancer as an unstoppable force, and while it remains one of humanity’s greatest challenges, discoveries like CPMV remind us that progress is being made. Every breakthrough, no matter how small, brings us closer to a world where the fear of cancer is replaced by hope, resilience, and healing. The plant virus that once only mattered to farmers is now being studied in some of the world’s most advanced laboratories, a journey that underscores how interconnected and surprising life truly is.
The broader lesson is this: solutions to our greatest challenges may not always come from where we expect. Sometimes they are hidden in plain sight, waiting for us to notice, to ask the right questions, and to persist long enough to uncover their potential. Just as the cowpea mosaic virus reawakens the immune system, discoveries like this reawaken our collective belief in the power of science, nature, and human ingenuity to change the world.
As you reflect on this, ask yourself: where in your own life are you overlooking simple, unexpected sources of strength? What possibilities might lie hidden in the ordinary, waiting to be discovered? The story of CPMV is not just about fighting cancer — it is about expanding the boundaries of what we believe is possible. And that, perhaps, is the most powerful medicine of all.
Loading...

