New Study Warns COVID-19 And Flu Might Awaken Dormant Cancer Cells In The Lungs

For decades, cancer research has been haunted by a mystery. Patients who had seemingly won the battle tumors eradicated, remission declared, health restored would sometimes face a shocking recurrence many years later. These weren’t always new cancers, but rather the old disease reappearing in unexpected places, long after the danger seemed gone. Scientists eventually realized the culprit was not fate or failure of treatment but something more elusive: dormant cancer cells. These quiet remnants of disease lodge themselves in distant tissues like the lungs, bones, or liver, where they lie hidden, invisible to scans and untouched by chemotherapy. They are like sleeping seeds scattered across the soil of the body, sometimes never sprouting, sometimes bursting into life when conditions shift. Until recently, the trigger that nudged these sleeping cells back into growth was unclear.
Now, new research has uncovered a surprising and unsettling answer. Common respiratory infections, such as influenza and COVID-19, appear capable of waking dormant breast cancer cells and sparking metastasis in the lungs. Mouse experiments reveal that viruses themselves are less the villains than the inflammation they provoke, which stirs the body into a state of chaos that provides fertile ground for hidden cancer cells. Human health records show a similar pattern: cancer survivors who contracted COVID were more likely to face cancer recurrence or death compared to those who avoided the infection. The findings invite us to rethink remission, survivorship, and the hidden conversations between immunity, infection, and disease. Yet they also open a door to new strategies of prevention and a deeper reflection on what it means for something once dormant to awaken whether in the body, the psyche, or the spirit.
Dormant Cancer Cells: The Hidden Embers
To understand why viruses matter, we must first explore the nature of dormant cancer cells. Unlike actively dividing tumor cells, which grow visibly and wreak havoc, dormant cells live in a suspended state, neither multiplying nor dying. They spread early in a cancer’s development, slipping quietly into far-off tissues. Many will remain permanently asleep, posing no threat. But a subset retain the potential to reignite years, even decades, after the original cancer was treated.
Researchers call these disseminated cancer cells (DCCs). They are like the embers of a long-extinguished fire, smoldering unseen beneath the ashes. Traditional therapies often miss them because chemotherapy and radiation target dividing cells, not quiet ones. This makes dormancy both a blessing and a curse: on one hand, the cells do not immediately cause harm; on the other, they create a latent risk, a hidden vulnerability that can transform remission into a precarious balance rather than a permanent victory.
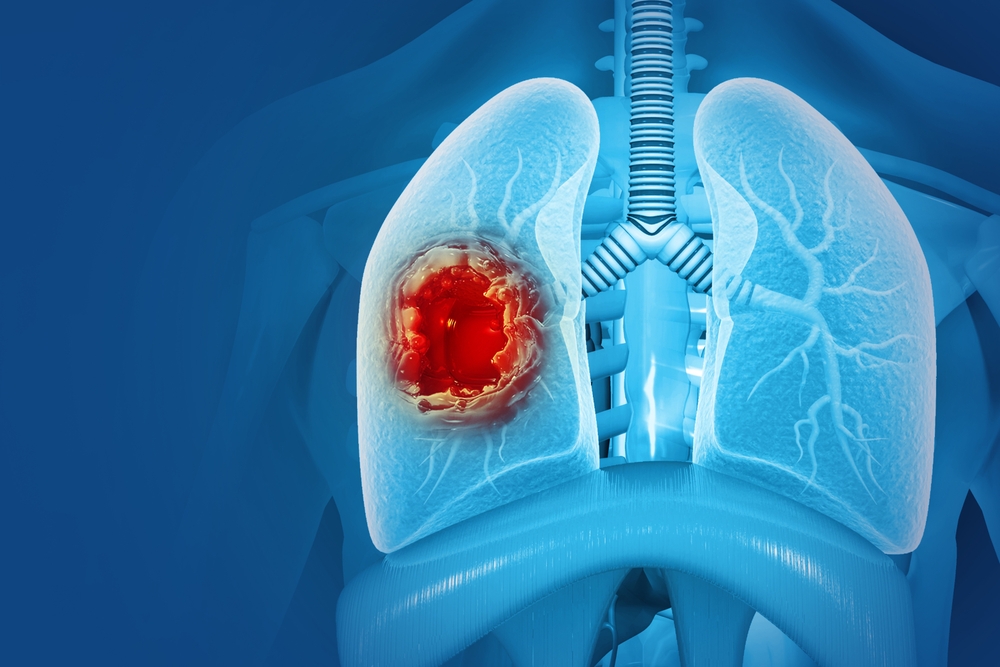
The lungs are particularly common resting grounds for these hidden seeds. The tissues are rich in blood flow and immune activity, making them a frequent destination for DCCs shed by breast cancers. In most survivors, these seeds stay silent. Yet under the right conditions a surge of inflammation, a change in immune surveillance they can awaken, multiply, and form metastatic tumors. The new studies show that viral infections like influenza and COVID may act as the sparks that fan these embers into flame.
From a spiritual perspective, this concept resonates with the way old traumas or shadow patterns sometimes resurface after years of quiet. Just as dormant cells lurk unseen, parts of our psyche hold onto unprocessed wounds. A sudden life event stress, illness, upheaval can act as the “infection” that awakens what we thought was resolved. The biology of cancer dormancy thus mirrors a universal truth: what lies sleeping is not necessarily gone, only waiting.
Viruses As Accidental Arsonists
So how can something as ordinary as the flu or COVID wake up cancer cells that had been quiet for years? The answer lies in inflammation. When the body detects an invader like a virus, it calls upon the immune system to mount a defense. Cells release a storm of signaling molecules, summoning reinforcements and creating an environment hostile to the pathogen. One of these molecules, interleukin-6 (IL-6), plays a central role.
In normal contexts, IL-6 is protective. It helps recruit immune cells to fight off infection and heal damaged tissues. But in the studies conducted at the University of Colorado and beyond, IL-6 also served as the very switch that jolted dormant breast cancer cells into action. In mouse models, when researchers disabled IL-6 signaling, viral infections no longer triggered the explosive growth of DCCs. In laboratory organoids tiny, lab-grown miniatures of human tissue exposure to IL-6 alone was enough to drive expansion. This makes IL-6 both healer and instigator: essential for fighting infection, yet dangerous for those harboring sleeping cancer cells.
The immune system’s role is even more complicated. CD8+ T cells, often called “killer T cells,” are natural defenders against both viruses and cancer. Yet during viral infection, CD4+ helper T cells can interfere, suppressing CD8 activity in a way that unintentionally shields cancer cells from attack. In effect, the immune system’s attempt to balance itself creates a window of vulnerability a few days or weeks when cancer’s hidden embers can flare.
This paradox highlights a deeper truth about biology: the same forces that protect us can, under different circumstances, betray us. It is not a battle of good versus evil but a dance of shifting roles, where context matters. From a symbolic perspective, viruses become less like malicious intruders and more like accidental arsonists, kicking up winds that stir old embers into flame. They are reminders that nothing in nature is one-sided, and that survival depends on harmony as much as defense.
Evidence From Humans: Patterns In The Data

Animal models provide controlled insight, but do these mechanisms hold true for humans? To test this, researchers turned to large health databases. In the UK Biobank, which tracks medical records of hundreds of thousands of people, those with prior cancer who contracted COVID before vaccines became available were nearly twice as likely to die of cancer compared to those who did not. Similarly, in the Flatiron Health database, which includes data from more than 36,000 breast cancer patients in the U.S., survivors who tested positive for COVID were about 40–50% more likely to develop lung metastases.
These numbers are striking, but they come with caveats. Correlation does not prove causation. Other factors delayed cancer care during the pandemic, general health vulnerabilities, or socioeconomic disparities could play a role. Still, when the patterns in human data line up with mechanisms demonstrated in mice, the likelihood that infection contributes directly becomes harder to ignore.
Perhaps the most telling feature is timing. Both in mice and in human records, the surge in cancer risk seemed to cluster within months or a couple of years after infection, suggesting a window of vulnerability tied to inflammation and immune disruption. Over time, the effect seemed to diminish. This aligns with the metaphor of embers: a gust of wind makes them flare, but once the wind dies down, some may smolder again rather than continue blazing. The danger lies not in one flare-up alone but in the cumulative effect of repeated infections, each adding fuel to the hidden fire.
For survivors, the data underline an uncomfortable truth: remission is not the same as finality. Even in apparent health, the body carries its history forward, and infections may shape the trajectory of that history in unseen ways. From a broader lens, this challenges how we think about healing not as a clean slate, but as an ongoing relationship with both the past and present.
Vaccines, Treatments, And New Strategies

The findings are sobering, but they are not without hope. If respiratory viruses can awaken dormant cancer cells, then strategies that prevent or blunt infections become powerful tools in survivorship care. Vaccination, long recommended for general health, now takes on added weight. COVID and flu vaccines reduce both the likelihood of infection and, crucially, the severity of disease. Milder infections generally mean less inflammation, which may translate into fewer sparks for dormant cells.
Beyond vaccines, antiviral drugs offer another line of defense. Rapid treatment of COVID with medications like Paxlovid, or influenza with Tamiflu, may shorten infection duration and reduce immune system upheaval. While these therapies were designed for acute benefit, they may also carry hidden long-term value for those at risk of recurrence.
The IL-6 connection is especially promising. Drugs that block IL-6 or its receptor already exist and are used in conditions such as rheumatoid arthritis, Castleman’s disease, and severe COVID. These medicines might one day be deployed to protect cancer survivors during respiratory infections, preventing the surge that wakes dormant cells. However, clinical trials are needed to balance the risks of suppressing immune responses with the potential benefit of guarding against metastasis.
From a lifestyle perspective, the findings also renew the importance of general health measures. Wearing masks in crowded indoor spaces, practicing good hygiene, and prioritizing rest and nutrition during respiratory virus season can serve not only as short-term safeguards but as acts of long-term resilience. For those who carry the hidden embers of disease, these steps are less about paranoia and more about tending the delicate balance of survival.
What This Could Mean For Cancer Survivors
While the idea that common respiratory viruses can reawaken dormant cancer cells is unsettling, it also offers survivors actionable knowledge. Awareness is power, and there are steps individuals can take to protect themselves and reduce potential risks:
- Stay current with vaccinations. COVID-19 boosters and annual flu shots are more than short-term protections. By reducing the severity of infections, they may also limit the inflammatory surges that could awaken dormant cancer cells.
- Treat infections quickly. At the first sign of COVID or flu, contacting a healthcare provider about antiviral options (such as Paxlovid or Tamiflu) may shorten illness and reduce immune overactivation.
- Be extra vigilant after serious illness. Survivors who experience a strong respiratory infection may want closer monitoring in the months that follow. Extra scans, bloodwork, or check-ins with an oncologist could provide early warning if anything begins to shift.
- Support the immune system naturally. Rest, sleep, nutrition, stress reduction, and moderate movement all help regulate immune balance. A resilient system is less likely to spiral into extreme inflammation.
- Consider masks and hygiene during high-risk seasons. For survivors, a mask in crowded indoor settings isn’t just about avoiding discomfort it could be about safeguarding long-term health.
These measures are not about living in fear, but about practicing vigilance and self-care. Just as cancer treatment itself required proactive choices, survivorship does too. By understanding the science and taking practical precautions, survivors can tilt the balance toward resilience and long-term health.
Dormancy, Awakening, And The Spiritual Mirror
Science speaks in the language of cytokines and cell types, but the symbolism of this discovery is rich with meaning. Dormant cancer cells resemble unresolved energies in the human psyche old wounds, traumas, or patterns of behavior that we imagine gone but which linger beneath the surface. Like the lungs holding onto hidden seeds of disease, our consciousness can harbor quiet shadows that rest until stirred by stress, upheaval, or illness.
Viruses, then, become metaphors for disruption. They remind us that balance is fragile, that the unseen currents of inflammation can awaken what we thought buried. Just as infections can reignite cancer, so too can moments of turmoil reawaken emotional scars we assumed were healed. Healing, whether cellular or spiritual, is not simply about eliminating the problem but cultivating resilience building an inner terrain where sparks find no fuel.
The metaphor of embers resonates across traditions. In Taoist philosophy, balance between yin and yang keeps the fire in harmony. In Jungian psychology, the shadow must be integrated, not ignored, to prevent its destructive reemergence. Even in spiritual practices of purification, the theme repeats: old energies must be acknowledged and transformed, not merely buried. The biology of dormancy offers a reminder that ignoring what lies beneath is never enough whether in the body or in the soul.
Keeping The Embers Cold
The revelation that flu and COVID can reawaken dormant breast cancer cells is a profound shift in how we view both infection and remission. It blurs the line between short-term illness and long-term survivorship, showing how deeply interwoven the immune system, environment, and cancer truly are. For survivors, the message is not one of fear but of awareness: vaccines, treatments, and preventive measures are not luxuries but essential shields in the ongoing journey of healing. For researchers, the discovery opens new pathways toward therapies that may one day keep dormant cells permanently silent.
On a broader level, the science reflects a universal truth. Dormancy and awakening are part of every cycle, whether in cells, ecosystems, or human consciousness. The past does not vanish; it lingers, shaping the future in ways both subtle and dramatic. By understanding these cycles, we gain the wisdom to live more fully caring for our bodies, tending our spirits, and honoring the delicate embers that flicker within us.
Loading...

