A Lab In Japan Grew Fully Functional Human Skin With Working Sweat Glands For Burn Victims

Something impossible just happened in a laboratory outside Kobe, Japan. Scientists watched as cells they’d carefully cultivated began organizing themselves into structures that shouldn’t exist outside a developing embryo. Hair follicles formed. Sweat glands appeared. Oil-producing organs took shape. Within weeks, what started as a cluster of reprogrammed cells became something medical science had chased for decades but never achieved.
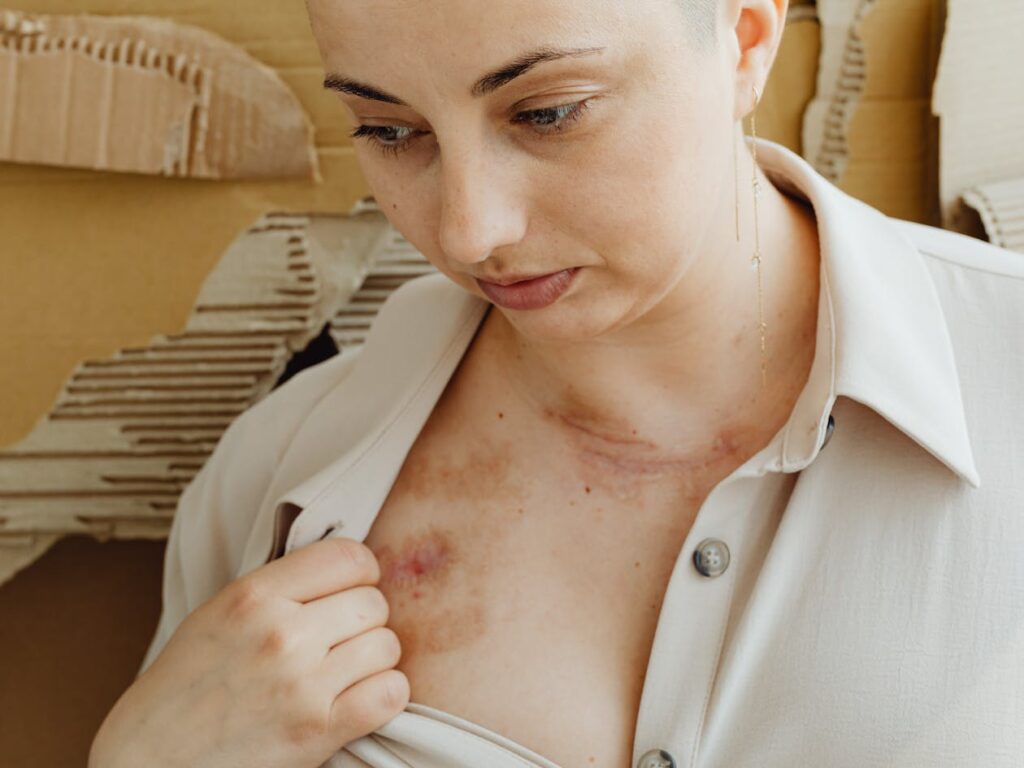
Burn victims worldwide face a cruel reality after surviving their injuries. Current treatments save lives but leave patients trapped in bodies that no longer function correctly. Artificial skin grafts provide basic coverage yet lack essential components that make skin actually work as living tissue. People spend lifetimes applying moisturizers, avoiding temperature extremes, and living with lost sensation where nerves once connected.
Japanese researchers at RIKEN Center for Developmental Biology just shattered those limitations. Their breakthrough, published in Science Advances, represents more than incremental progress. Something fundamentally different emerged from their petri dishes and transplantation experiments.
Japanese Scientists Just Solved Burn Victim’s Biggest Problem

Dr. Takashi Tsuji led his research team through years of experiments testing different approaches to growing functional skin tissue. Success finally came when they developed novel transplantation methods using induced pluripotent stem cells. Laboratory results showed formation of complete three-dimensional skin organ systems containing every structure found in natural skin.
Medical community reactions ranged from excitement to disbelief when reviewing published findings. Previous attempts at bioengineering skin produced flat sheets of epithelial cells lacking the complexity required for full organ function. Tsuji’s team achieved what many considered theoretically possible but practically unattainable.
Published data confirmed presence of all three skin layers, plus hair follicles, sebaceous glands, sweat glands, and subcutaneous fat tissue. Mouse experiments demonstrated these laboratory-grown tissues could be successfully transplanted and would integrate with host nervous systems and muscle tissue.
Current Artificial Skin Falls Painfully Short
Existing skin graft technologies save lives following severe burns but create ongoing challenges for survivors. Patients receive sheets of cultured epithelial cells that form basic protective barriers yet miss critical functional components.
Sebaceous glands produce natural oils that keep skin moisturized and maintain waterproof properties. Without these structures, burn victims must apply lotions constantly to prevent grafted areas from drying out and cracking. Daily moisturizing routines become lifelong necessities.
Sweat gland absence means grafted skin cannot regulate body temperature through perspiration. Burn survivors struggle with overheating during physical activity or warm weather. Bodies lose major cooling mechanisms when skin grafts lack functional sweat glands.
Nerve connections fail to properly restore in current artificial skin. Sense of touch disappears in grafted regions, creating safety hazards and reducing quality of life. People can’t feel pressure, temperature changes, or pain signals that protect against injury.
Visual appearance of current grafts often doesn’t match surrounding natural skin. Color differences, texture variations, and obvious scarring cause psychological distress and social challenges for burn survivors dealing with visible disfigurement.
Skin Does Way More Than Just Cover Your Body
Skin represents our largest organ, performing complex functions that extend far beyond simple protective covering. Three distinct layers work together through coordinated biological processes that maintain health and enable environmental interaction.
Epidermis forms outermost barrier against pathogens, chemicals, and physical damage. Specialized cells continuously regenerate, replacing damaged tissue and maintaining protective function. Water retention and pathogen exclusion depend on intact epidermal structures.
Dermis contains blood vessels supplying nutrients, nerve endings providing sensory information, hair follicles enabling hair growth, and glands secreting oils and sweat. Middle layer houses most functional components that make skin an active organ rather than passive barrier.
Subcutaneous layer provides insulation through fat deposits, cushions internal structures from external impacts, and anchors skin to underlying muscle and bone. Deepest layer connects skin to rest of body while storing energy and regulating temperature.
Hair follicles, sebaceous glands, sweat glands, and nerve endings all contribute to skin’s remarkable capabilities. Losing these structures through burns or other injuries creates functional deficits that current medical treatments cannot fully address.
Stem Cells Hold Secret to Perfect Skin Replacement
Researchers extracted cells from mouse gums and exposed them to chemical cocktails that essentially turned back their developmental clocks. Adult cells transformed into induced pluripotent stem cells capable of becoming any cell type in the body.
iPS cells offer huge advantages over embryonic stem cells by avoiding ethical controversies while providing similar differentiation potential. Scientists can reprogram adult tissue samples into pluripotent states without destroying embryos or requiring controversial biological materials.
After several days in laboratory culture conditions, iPS cells formed three-dimensional structures called embryoid bodies. These clumps contained random mixtures of cell types that would appear in developing embryos, including precursors to skin tissue.
Breakthrough came from recognizing that proper organization requires more than just individual cells or single embryoid bodies. Tsuji’s team developed a clustering method that encased multiple embryoid bodies together in collagen gel before transplantation.
Cell signaling between adjacent embryoid bodies triggered self-organization processes similar to natural embryonic development. Without direct manipulation, cells began differentiating and arranging themselves into complex tissue structures following developmental blueprints encoded in their genetic programs.
Growing Skin Required Novel Transplant Technique
Traditional approaches attempted growing skin tissues entirely in laboratory culture dishes or transplanting single embryoid bodies into host animals. Both methods produced limited results lacking the complexity of functional skin organs.
Innovation involved creating clusters of approximately 30 to 48 embryoid bodies encased together in gel matrix, then transplanting entire clusters into subrenal capsules of immune-deficient mice. Kidney capsule location provided rich blood supply and protected environment for tissue development.
One month growth period allowed cells to differentiate and organize following natural developmental patterns. Regular monitoring tracked progress as three-dimensional structures emerged and matured within host animals.
Cellular analysis confirmed formation of complete integumentary organ systems after development period concluded. Researchers extracted grown tissues and performed detailed examinations of cellular structure, gene expression patterns, and functional capabilities.
Lab-Grown Skin Contains Every Missing Component

Microscopic examination revealed proper formation of epidermis, dermis, and subcutaneous fat layers arranged in correct anatomical relationships. All three major skin layers developed appropriate cellular composition and structural organization.
Hair follicles appeared throughout tissue samples, displaying proper orientation and depth within skin layers. Follicle structures included all necessary components for hair growth, including dermal papilla cells that regulate hair cycle and melanocytes that provide pigmentation.
Sebaceous glands formed adjacent to hair follicles in anatomically correct positions. Oil-producing structures showed appropriate cellular differentiation and glandular architecture needed for lipid secretion.
Sweat glands developed with proper coiled structures and ductal systems for perspiration excretion. Eccrine gland formation indicated potential for temperature regulation through evaporative cooling.
Subcutaneous adipose tissue provided cushioning and insulation layer beneath dermal structures. Fat deposits demonstrated appropriate cellular organization and lipid accumulation characteristic of natural subcutaneous tissue.
Transplanted Skin Actually Sprouted Hair
Researchers divided matured tissue into smaller pieces containing 10 to 20 follicular units and transplanted them onto backs of hairless nude mice using follicular unit transplantation techniques. Surgical methods mimicked approaches used in human hair restoration procedures.
Black hair emerged from transplanted follicles just 14 days after grafting surgery, despite recipient mice having white hair. Pigmentation proved melanocytes from original stem cells had properly differentiated and integrated into follicle structures.
Hair follicles made necessary connections with surrounding muscle tissue in host animals. Arrector pili muscles attached to follicles in correct anatomical arrangements, enabling hair to stand up in response to cold or emotional stimuli.
Nerve fibers from host mice grew into transplanted skin tissue and connected with follicle structures. Sensory innervation restored capability for hair follicles to detect external stimuli and respond appropriately through reflex pathways.
Follow-up observations over three months confirmed transplanted follicles underwent natural hair growth cycles. Anagen growth phases alternated with telogen resting phases in patterns matching normal mouse hair biology. Follicles demonstrated stem cell populations required for regenerating new hairs after old ones shed.
Science Behind Three-Layer Skin Creation

Epidermis developed through differentiation of epithelial progenitor cells into stratified squamous epithelium. Multiple cell layers formed with appropriate keratinocyte differentiation patterns creating protective barrier function.
Dermis emerged through mesenchymal cell organization into connective tissue matrix. Collagen and elastin fibers provided structural support while blood vessels and nerve fibers infiltrated from host tissues.
Subcutaneous layer formed through adipocyte differentiation and lipid accumulation in fatty tissue. Fat cells organized into lobules separated by connective tissue septa matching natural subcutaneous architecture.
Wnt10b signaling molecule played crucial role controlling hair follicle frequency and development. Chemical treatment with Wnt10b increased number of follicles forming in cultured tissues compared to untreated controls. Signaling pathway activation guided stem cells toward follicular differentiation pathways.
Lead researcher Dr. Takashi Tsuji explained the significance: “Up until now, artificial skin development has been hampered by the fact the skin lacked the important organs, such as hair follicles and exocrine glands, which allow the skin to play its important role in regulation. With this new technique, we have successfully grown skin that replicates the function of normal tissue.”
Burn Victims Could Finally Get Real Skin Back

Severe burn injuries destroy complex skin structures beyond body’s natural healing capabilities. Third-degree burns eliminate all skin layers including regenerative stem cell populations needed for spontaneous recovery.
Current treatment options include taking skin grafts from undamaged body areas, leaving patients with two injury sites requiring healing. Full-body burn victims lack sufficient donor sites for traditional grafting approaches.
Temperature regulation problems plague burn survivors lacking functional sweat glands. Exercise intolerance and heat sensitivity limit daily activities and employment options. Simple tasks become dangerous when bodies cannot properly dissipate excess heat.
Lost sensation creates safety risks burn survivors face constantly. Inability to feel pain warnings allows repeated injuries from hot surfaces, sharp objects, or excessive pressure. Protective feedback mechanisms disappear with damaged nerve connections.
Psychological trauma accompanies visible scarring and disfigurement from current artificial skin grafts. Social isolation, depression, and reduced quality of life follow severe burns even after physical wounds heal. Functional, natural-appearing skin restoration could address emotional healing alongside physical recovery.
Revolutionary Impact on Regenerative Medicine Field
Success growing functional skin proves broader concept that complex organs can be bioengineered from stem cells using proper developmental guidance. Methodology provides roadmap for other tissue engineering projects pursuing kidneys, livers, hearts, and other organs.
Self-organization capabilities demonstrated by stem cells exceed what researchers expected possible through laboratory manipulation. Cells contain intrinsic programs driving proper structure formation when placed in appropriate developmental contexts.
Opens possibilities beyond burn treatment into numerous medical applications. Cosmetics industry could test products on realistic lab-grown skin instead of animals. Pharmaceutical companies could screen drugs using human-relevant tissue models. Basic research gains new tools for studying skin biology and disease processes.
Japan continues leading world in regenerative medicine research through substantial government funding and collaborative initiatives. Multiple research groups pursue bioengineered teeth, salivary glands, and other tissues using similar stem cell approaches.
Journey from laboratory breakthrough to patient bedside treatment will take years of continued work. Yet this achievement represents genuine progress toward regenerative medicine dreams of growing replacement organs that restore full function to damaged bodies.
Loading...

