Scientists Discover How to Reverse Bone Loss at Any Age
Scientists at Leipzig University watched something remarkable happen in their laboratory. Mice with fragile, deteriorating bones received daily injections of a compound identified through computer screening. Within weeks, measurements showed dramatic changes. Bone density increased. Structural integrity improved. Animals that should have continued weakening instead grew stronger.
Decade-long investigation into mysterious cell receptors finally yielded breakthrough results. Published findings revealed molecular switches that control bone formation throughout life. Even more striking: researchers discovered ways to activate these switches artificially, reversing damage that conventional medicine considers irreversible.
Millions of people worldwide suffer bone loss as they age, facing fractures, disability, and reduced independence. Current treatments offer limited solutions plagued by serious side effects and diminishing returns. What German researchers uncovered could transform how medicine approaches bone health across entire lifespans.
German Scientists Just Cracked Aging Bone Code
Professor Ines Liebscher leads biochemistry research at Leipzig University’s Rudolf Schönheimer Institute. Her team spent over ten years investigating adhesion G protein-coupled receptors, relatively unexplored molecular structures that regulate numerous body functions. Among these receptors, GPR133 emerged as particularly important for bone density regulation.
Research findings published in Signal Transduction and Targeted Therapy documented GPR133’s central role in building and maintaining healthy bone tissue. Previous genome-wide association studies had linked genetic variations in GPR133 to differences in bone mineral density and body height across human populations. Yet precise mechanisms remained unclear until Liebscher’s team conducted detailed molecular investigations.
Collaborative work with researchers from Shandong University in China provided additional validation. International research center status at Leipzig gave teams access to specialized equipment and expertise needed for complex receptor studies. Years of careful experimentation finally revealed how GPR133 controls bone formation processes.
Six Million People Need Better Solutions Now
Germany alone counts approximately six million osteoporosis patients, predominantly women experiencing postmenopausal bone loss. Worldwide numbers reach tens of millions suffering from this progressive disease characterized by declining bone density and increased fracture risk.
Current medication options include bisphosphonates that prevent bone breakdown, hormone replacement therapies that carry cancer and blood clot risks, and parathyroid hormone treatments effective only for two years maximum. Side effects range from uncomfortable to dangerous. Jaw bone death, though rare, occurs with some bisphosphonates. Hormone therapies increase risks of breast cancer and thrombosis.
Many patients discontinue treatment due to adverse effects or loss of efficacy over time. Medical community recognizes urgent need for safer alternatives that maintain effectiveness through long-term use. New therapeutic targets represent crucial steps toward better options with fewer complications.
Hidden Receptor Controls Bone Density Throughout Life
Cell surfaces contain numerous receptor proteins that function as molecular switches. When specific molecules bind to these receptors, internal signaling cascades activate, triggering various cellular responses. G protein-coupled receptors represent largest receptor family, with many serving as pharmaceutical drug targets.
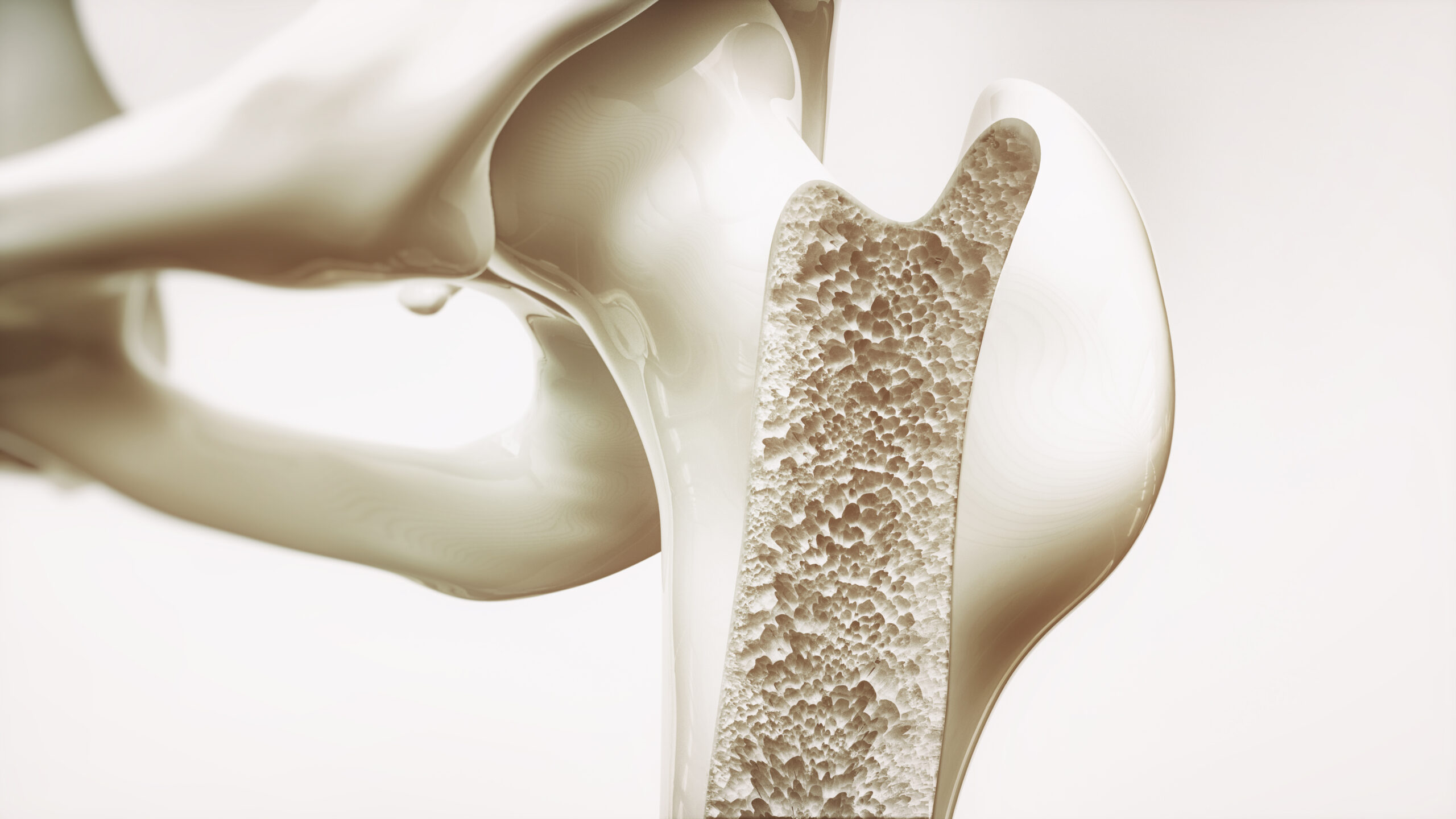
GPR133 belongs to adhesion GPCR subfamily, characterized by complex structures including domains that respond to mechanical forces and cell-cell interactions. Located on bone-forming osteoblast surfaces, GPR133 receives signals from neighboring cells and responds to physical strain from weight-bearing activities.
Receptor activation triggers internal biochemical pathways involving cyclic adenosine monophosphate and β-catenin signaling. These pathways control osteoblast differentiation, maturation, and bone-building activities. Genetic variations affecting GPR133 function correlate with osteoporosis risk, suggesting receptor plays decisive role in maintaining skeletal strength.
Knockout Mice Revealed Devastating Bone Loss Pattern
Genetic engineering techniques allowed researchers to create mice completely lacking functional GPR133 genes. Both constitutive knockouts (missing gene everywhere) and osteoblast-specific knockouts (missing gene only in bone-forming cells) showed similar phenotypes.
Young animals developed osteoporosis-like symptoms rapidly despite normal diet and activity levels. Bone density measurements revealed significantly reduced cortical thickness and trabecular number compared to normal mice. Microscopic analysis showed fewer osteoblasts present and reduced bone formation rates.
Professor Ines Liebscher explained the findings: “If this receptor is impaired by genetic changes, mice show signs of loss of bone density at an early age – similar to osteoporosis in humans.”
Three-point bending tests confirmed functional consequences. Bones from knockout animals broke more easily under mechanical stress despite seemingly modest density reductions. Even heterozygous mice carrying one functional and one non-functional gene copy showed intermediate phenotypes with measurable bone weakness.
AP503 Compound Switches On Bone Building Machinery
Computer-assisted virtual screening examined thousands of potential molecules for ability to activate GPR133 receptors. AP503 emerged as highly specific agonist that selectively stimulates GPR133 without affecting other receptor types.
Small molecule structure allows AP503 to bind GPR133 and mimic natural activation normally triggered by cell-cell contact and mechanical forces. Laboratory testing confirmed compound increases cyclic AMP levels inside osteoblasts, activating downstream signaling pathways that promote bone formation.
Liebscher’s team demonstrated AP503’s effectiveness: “Using the substance AP503, which was only recently identified via a computer-assisted screen as a stimulator of GPR133, we were able to significantly increase bone strength in both healthy and osteoporotic mice.”
Cell culture experiments showed AP503 enhanced osteoblast differentiation markers, increased alkaline phosphatase activity, and improved mineralization capacity. Compound worked through same pathways as natural receptor activation but could be administered therapeutically to boost bone formation beyond baseline levels.
Exercise and AP503 Create Powerful Bone Building Synergy

Mechanical loading from physical activity naturally activates GPR133 through forces transmitted across bone tissue. Research team designed experiments combining treadmill running with AP503 treatment to test whether these stimuli worked additively or synergistically.
Control mice remained sedentary without drug treatment. Exercise-only group ran on treadmills following progressive training protocol. AP503-only group received daily injections without exercise. Combination group experienced both interventions simultaneously.
Results showed clear synergistic effects. Exercise alone improved bone volume and trabecular number. AP503 alone increased bone volume, trabecular thickness, and trabecular number. Combined treatment produced significantly better results than adding individual effects would predict.
Three-point bending tests revealed combination therapy created strongest bones, able to withstand highest loads before breaking. Mechanism likely involves partial receptor activation from either stimulus alone, while combined approach provides more complete activation driving maximal bone formation response.
Two Critical Pathways Coordinate Bone Formation
Molecular analysis revealed GPR133 controls osteoblast function through coordinated activation of two essential signaling systems. First, receptor stimulation increases cyclic AMP production through Gs protein activation. Elevated cyclic AMP activates protein kinase A, which affects numerous cellular processes.
Second, GPR133 signaling influences β-catenin pathway known for roles in bone development and remodeling. Normally, glycogen synthase kinase-3 phosphorylates β-catenin, marking it for degradation. Protein kinase A activation from cyclic AMP elevation interferes with this phosphorylation, stabilizing β-catenin levels.
Higher β-catenin concentrations drive expression of genes controlling osteoblast differentiation and function. Cells produce more collagen, alkaline phosphatase, osteocalcin, and other proteins essential for bone matrix formation and mineralization.
Receptor-deficient cells showed dramatically reduced levels of both cyclic AMP and β-catenin. Adding compounds that bypass receptor and directly elevate cyclic AMP restored β-catenin levels and rescued bone formation capacity, confirming pathway connections.
Bone Builders Multiply While Destroyers Slow Down

Healthy bone maintenance requires balance between osteoblasts building new tissue and osteoclasts breaking down old or damaged bone. GPR133 activation shifts this balance favorably through multiple mechanisms.
Direct effects on osteoblasts include increased cell numbers, enhanced differentiation, and improved function. Activated osteoblasts produce more bone matrix proteins and mineralize tissue more effectively. Gene expression analysis showed elevated markers of mature, active osteoblasts.
Indirect effects on osteoclasts occur through altered communication between cell types. Osteoblasts secrete osteoprotegerin, which blocks receptor activator of nuclear factor kappa-B ligand from stimulating osteoclast formation. GPR133-deficient mice showed reduced osteoprotegerin levels, allowing excessive osteoclast activation.
Additional evidence suggests GPR133 expression in osteoclasts themselves, where receptor activation may directly inhibit bone resorption activities. Combined effects create comprehensive shift toward net bone gain rather than loss.
Mice Bones Grew Stronger Within Four Weeks
Treatment experiments used young mice receiving daily AP503 injections for four weeks. Microcomputed tomography scans documented structural changes with high precision. Bone volume to total volume ratios increased significantly in treated animals compared to vehicle-injected controls.
Trabecular bone parameters improved across multiple measurements. Number of trabecular struts increased. Individual trabeculae grew thicker. Spacing between struts decreased as bone filled previously empty regions. Cortical bone showed increased thickness and density.
Calcein fluorescent labeling tracked new bone formation rates. Treated mice showed broader bands of newly mineralized tissue compared to controls, confirming accelerated bone deposition. Histological analysis revealed more numerous osteoblasts along bone surfaces.
Biomechanical testing validated functional improvements. Femurs from treated mice tolerated higher loads before fracturing. Elastic modulus measurements indicated stiffer, more resistant bone tissue capable of better withstanding daily mechanical stresses.
Osteoporotic Mice Completely Reversed Bone Loss

Ovariectomy surgery removes ovaries, eliminating estrogen production and mimicking postmenopausal hormonal changes that trigger rapid bone loss in women. Female mice underwent surgery at eight weeks age, followed by four-week recovery period allowing bone deterioration.
Vehicle-treated ovariectomized mice showed expected osteoporotic changes: reduced bone volume, decreased mineral density, thinner cortical and trabecular bone, increased trabecular spacing. Sham-operated controls receiving fake surgery maintained normal bone parameters.
Daily AP503 injections for four weeks substantially reversed osteoporotic changes. Bone volume, mineral density, cortical thickness, and trabecular number all improved dramatically compared to vehicle-treated ovariectomized mice. Many parameters returned nearly to sham-operated levels.
Cellular analysis showed AP503 restored normal osteoblast and osteocyte numbers while reducing excessive osteoclast populations. Proof-of-concept demonstration confirmed treatment works for established disease, not just prevention. Results suggest potential for reversing existing osteoporosis in human patients.
Muscle Strength Bonus Amplifies Treatment Benefits

Earlier research from same Leipzig group investigated GPR133 effects on skeletal muscle tissue. Published findings showed AP503 treatment also strengthens muscle fibers, improving contractile force and endurance capacity.
Dr. Juliane Lehmann, lead author and researcher at Rudolf Schönheimer Institute, emphasized broader implications: “The newly demonstrated parallel strengthening of bone once again highlights the great potential this receptor holds for medical applications in an aging population.”
Dual effects address two interconnected problems contributing to frailty and fracture risk among elderly populations. Weak bones break easily during falls. Weak muscles increase fall likelihood and reduce ability to catch oneself. Strengthening both systems simultaneously provides comprehensive protection.
Combined bone and muscle benefits could prove especially valuable for bedridden patients recovering from surgery or illness. Immobility causes rapid deterioration of both tissues. Treatment might prevent or reverse damage during extended bed rest periods.
From Laboratory Discoveries to Patient Treatments
Bones/Muscles Strenght Breakthrough
— Dr Singularity (@Dr_Singularity) July 29, 2025
Exciting breakthrough from Leipzig University.
Scientists discovered that activating a key receptor, GPR133, supercharges bone and muscle strength. Using a powerful compound called AP503, they boosted bone density in mice, even those with… pic.twitter.com/7Hau1TNRNa
Mouse model successes represent crucial early steps, yet substantial work remains before human clinical applications. Species differences in bone physiology mean results don’t automatically translate. Safety testing requires extensive evaluation across multiple animal species before human trials begin.
Dose-finding studies must determine optimal treatment levels balancing efficacy against potential side effects. Pharmacokinetic analysis tracks how bodies absorb, distribute, metabolize, and eliminate drugs. Long-term toxicity studies assess risks from extended exposure.
Regulatory approval processes demand rigorous documentation of safety and effectiveness. Phase I trials test safety in small healthy volunteer groups. Phase II trials evaluate efficacy in patient populations. Phase III trials compare new treatments against existing standards across large populations.
Realistic timeline estimates suggest 5-10 years minimum before AP503 or similar compounds reach clinical use. Manufacturing scale-up, quality control systems, and distribution networks require substantial investment and development time.
Yet breakthrough nature of GPR133 discovery justifies optimism about eventual translation. Receptor-based approach offers advantages over current osteoporosis treatments. Working through natural bone-building pathways may produce fewer side effects than drugs that simply block bone breakdown.
Genetic screening could identify individuals carrying GPR133 mutations predisposing them toward early osteoporosis. Preventive treatment before significant bone loss occurs might preserve skeletal health throughout lifespans. Personalized medicine approaches could target interventions toward those most likely to benefit.
Applications extend beyond typical osteoporosis patients. Astronauts experiencing rapid bone loss during space missions could benefit from treatments compensating for lack of gravitational loading. Combination with structured exercise programs might allow lower drug doses while achieving better outcomes through synergistic effects.
Discovery opens new chapter in bone health research while acknowledging remaining challenges. Pathway from laboratory breakthroughs to bedside treatments follows long but increasingly well-defined route. Millions suffering progressive bone loss now have reason to hope for fundamentally better therapeutic options in coming years.
Loading...

