For decades, lupus has been one of medicine’s most puzzling and emotionally charged mysteries. It is a disease that can quietly simmer for years before suddenly flaring, attacking the body from the inside out, leaving patients exhausted, in pain, and often searching for answers that never quite come. Scientists have long suspected that something external was pulling the strings behind this autoimmune disorder, but until recently, they could not prove exactly what.
Now, new research suggests that the answer may have been with us all along.
A virus carried by more than 95 percent of adults worldwide may be directly responsible for triggering lupus. Even more striking, scientists say they finally understand how it happens. After years of indirect clues and unanswered questions, researchers believe they have identified the biological chain reaction that turns a common childhood infection into a life-altering autoimmune disease.
This discovery does not just help explain lupus. It may fundamentally change how scientists think about autoimmune illness as a whole.
The Virus Almost Everyone Has
The Epstein-Barr virus, commonly known as EBV, is one of the most widespread viruses on Earth. It spreads through saliva and is often picked up in childhood through everyday interactions like sharing cups or utensils, or later in adolescence through close contact such as kissing.
For many people, EBV causes few noticeable symptoms. Some develop mononucleosis, marked by fever, sore throat, and intense fatigue that can last weeks or even months. But for the vast majority, the virus slips into the body quietly and stays there for life.
Once infected, there is no way to fully eliminate EBV. Instead, it takes up permanent residence inside certain immune cells, entering a dormant state where it largely avoids detection. For decades, this dormancy led scientists to believe that EBV was mostly harmless after the initial infection passed.
What researchers are now realizing is that dormant does not mean inactive.
What Lupus Does to the Body

Lupus, formally known as systemic lupus erythematosus, is a chronic autoimmune disease. Instead of protecting the body, the immune system mistakenly attacks healthy tissues and organs. The result can be widespread inflammation and damage affecting the skin, joints, kidneys, heart, lungs, blood cells, and even the brain.
Symptoms vary dramatically between individuals. Some experience persistent fatigue, joint pain, and skin rashes. Others develop severe complications such as kidney failure, heart inflammation, or neurological problems. This variability has made lupus notoriously difficult to diagnose and treat.
Globally, an estimated five million people live with lupus. In the United States alone, estimates range from several hundred thousand to over a million. Roughly nine out of ten patients are women, a pattern scientists still struggle to fully explain.
While modern treatments can help manage symptoms and slow disease progression, there is no cure. For a small but significant percentage of patients, lupus can be life-threatening.
A Long-Suspected Connection
The idea that viruses might trigger autoimmune diseases is not new. For years, researchers noticed that nearly all people diagnosed with lupus had previously been infected with EBV. That observation alone was not enough to prove causation, especially given how common the virus is.
If nearly everyone carries EBV, why do only a small fraction develop lupus?
This question haunted immunologists for decades. They knew the virus was present, but they could not explain how it might transform a normal immune response into a self-destructive one. The missing piece was a clear mechanism showing how EBV could hijack immune cells in a way that specifically led to lupus.
That is where the new Stanford-led research comes in.
Inside the Immune System’s Weak Spot
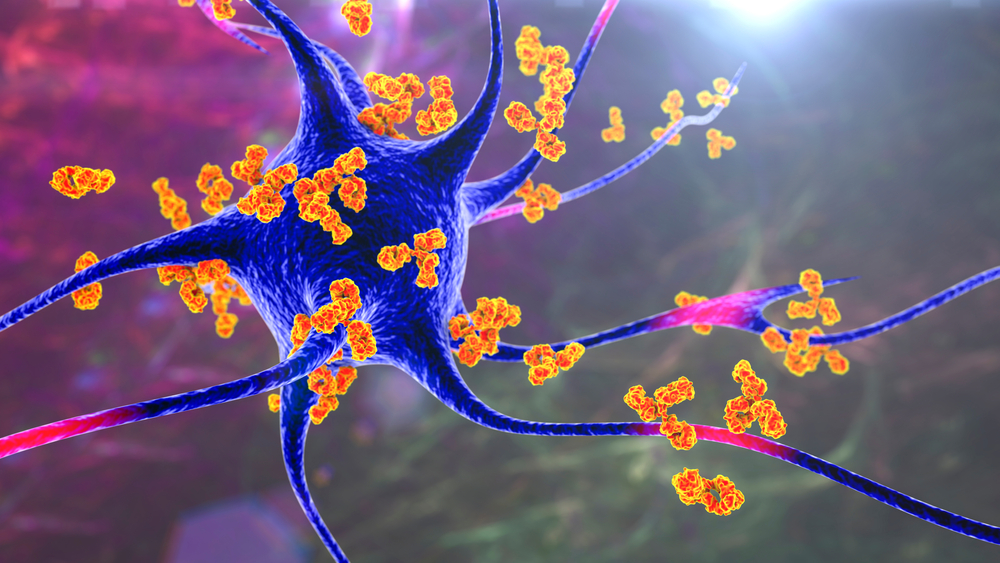
To understand the breakthrough, it helps to look at a specific type of immune cell called a B cell. B cells play a central role in defending the body. They produce antibodies that recognize and bind to invading pathogens, helping neutralize threats like bacteria and viruses.
B cells also act as messengers. They present fragments of pathogens to other immune cells, effectively sounding the alarm and coordinating a larger immune response.
But there is a catch.
Because B cells generate their antibody diversity through a random process, about 20 percent of them are naturally capable of recognizing the body’s own tissues. These self-reactive B cells are usually kept in check, held in an inactive state so they do not cause harm.
Lupus begins when those safeguards fail.
A Technological Breakthrough

For years, scientists struggled to study EBV inside B cells because the virus hides so effectively. In healthy individuals, fewer than one in 10,000 B cells carries the virus, making infected cells extremely difficult to identify.
Researchers at Stanford Medicine developed an ultra-sensitive sequencing technique that allowed them to pinpoint exactly which B cells were infected and analyze which genes were being activated inside them. This technology made it possible to observe interactions that were previously invisible.
When scientists applied this method to samples from lupus patients, the difference was striking.
In people with lupus, about one in 400 B cells was infected with EBV, a 25-fold increase compared to healthy individuals. That alone was significant. But the real revelation came when researchers examined what those infected cells were doing.
The Molecular Switch That Changes Everything
Even when EBV is dormant, it occasionally prompts the infected B cell to produce a viral protein known as EBNA2. This protein acts like a molecular switch, turning on genes that would normally remain silent.
The researchers discovered that EBNA2 activates a cascade of inflammatory genes inside the B cell. Some of these genes produce proteins that further amplify immune signaling, effectively transforming the B cell into a powerful antigen-presenting cell.
In simple terms, EBV turns infected B cells into immune system amplifiers.
These reprogrammed cells then activate helper T cells, which go on to recruit large numbers of other immune cells, including dormant self-reactive B cells and aggressive killer T cells. Once this chain reaction begins, it no longer matters whether the newly recruited cells are infected with EBV.
The immune system has been set on a destructive path.
How Lupus Takes Hold
As the immune response escalates, self-reactive B cells begin producing antinuclear antibodies. These antibodies target components found inside the nuclei of the body’s own cells.
Because nearly every cell in the body contains a nucleus, the damage caused by these antibodies can be widespread and unpredictable. Organs far removed from the initial immune trigger can become inflamed and injured.
This explains why lupus can affect so many different systems and why symptoms can shift over time. It also helps clarify why the disease can flare unpredictably, sometimes after long periods of relative calm.
According to the researchers, this EBV-driven cascade may be the central event that initiates lupus in susceptible individuals.

Why Most People Do Not Get Lupus
One of the most important questions remains unanswered. If EBV is nearly universal, why do so few people develop lupus?
Scientists believe the answer likely involves a combination of factors.
One possibility is that only certain strains of EBV have the ability to activate B cells in this dangerous way. Another is that genetic differences in immune regulation make some people more vulnerable to the virus’s effects.
Researchers also suspect that EBV must infect a very specific subset of B cells, namely the self-reactive ones, in order to trigger lupus. If the virus infects other B cells instead, the cascade may never begin.
In short, two rare events may need to coincide. The right virus strain must infect the right immune cells in a genetically susceptible person.
Beyond Lupus
The implications of this discovery extend far beyond lupus alone.
EBV has already been linked to other autoimmune diseases, including multiple sclerosis, rheumatoid arthritis, and Crohn’s disease. In several of these conditions, scientists have detected signs of the same EBNA2-driven gene activation seen in lupus.
If similar mechanisms are confirmed, it could mean that a single virus plays a role in triggering multiple autoimmune disorders. This does not mean EBV inevitably causes disease. Rather, it suggests that under certain conditions, the virus can tip the immune system into a self-destructive state.
Understanding that process could open the door to entirely new ways of preventing and treating autoimmunity.
What This Means for Treatment
Current lupus treatments focus largely on suppressing the immune system. While these drugs can reduce symptoms and prevent organ damage, they also leave patients more vulnerable to infections and other complications.
The new findings point toward more targeted strategies.
One promising approach involves deeply depleting B cells, effectively removing both EBV-infected cells and self-reactive cells from circulation. Over time, the body replaces them with new B cells generated in the bone marrow, which are free of the virus.
Early evidence suggests that some patients who undergo deep B cell depletion experience long-term remission, even without continued medication. Researchers are now investigating whether this remission occurs because the EBV-driven driver cells have been eliminated.
If confirmed, it could represent a major shift in lupus therapy.

The Promise and Limits of Vaccines
The findings also strengthen the case for developing an EBV vaccine.
Several vaccine candidates are already in early clinical trials. In theory, preventing EBV infection could reduce the risk of developing lupus and possibly other autoimmune diseases.
However, there is a catch. EBV infection usually occurs early in life, meaning a vaccine would likely need to be administered in infancy to be effective. Vaccines cannot eliminate the virus once infection has already occurred.
Still, even partial protection could have enormous public health benefits.
A Turning Point in Autoimmune Research
For decades, lupus patients have lived with uncertainty about why their immune systems turned against them. The idea that a nearly universal virus could be responsible has always been unsettling, but now it comes with clarity.
For the first time, scientists can trace a clear biological pathway from a common infection to a devastating disease. That understanding does not assign blame, nor does it offer instant cures. But it does provide something equally important.
It offers answers.
By revealing how Epstein-Barr virus can reprogram immune cells and ignite autoimmunity, researchers have taken a major step toward unraveling one of medicine’s longest-standing mysteries. The hope is that this knowledge will lead to more precise treatments, better prevention strategies, and ultimately, a future where lupus is no longer a lifelong sentence.
For millions of people living with the disease, that possibility alone is transformative.
Loading...

