Brain Stimulation Technique Shown to Help Repair Neuron Communication Tied to Memory Decline in Alzheimer’s Disease

Every three seconds, somewhere in the world, a person drifts a little further away from their memories. A familiar name slips from reach, a childhood story dissolves mid-sentence, a once-clear face blurs into uncertainty. This is the cruel arithmetic of Alzheimer’s disease a condition that quietly rewrites the brain’s wiring until the very connections that define us begin to fail.
For decades, science has searched for ways to slow this unraveling. Most available drugs offer only modest relief, often at the cost of serious side effects. They treat symptoms, but they don’t mend the broken lines of communication between neurons. What if, instead of simply patching the leaks, we could restore the conversation itself?
Think of the brain as a bustling city. In Alzheimer’s, the streets aren’t destroyed outright, but the traffic lights fail, intersections get jammed, and signals never reach their destination. Neurons still exist but they’re cut off from one another. Now researchers are experimenting with ways to flip the switches back on, using gentle pulses of magnetic or electrical energy to reignite the dialogue.
The early results are striking. Small studies suggest that brain stimulation can help neurons “talk” again, slowing memory decline and preserving daily function. It is not a cure, but it is a new kind of hope one that focuses on repairing the conversation of the brain, not just fighting the debris.
Why Neurons Stop Talking
Memory isn’t stored in one place like files on a hard drive. It’s written into the living connections between neurons, the brain’s billions of messengers. These connections, called synapses, aren’t static. They strengthen, weaken, or disappear altogether depending on how often we use them. This constant reshaping synaptic plasticity is what allows you to recall a loved one’s laugh, learn a new language, or forget a bad day.
In Alzheimer’s disease, that flexibility erodes long before brain cells die in large numbers. The problem begins with toxic proteins beta amyloid and tau that build up inside and around neurons. These proteins interfere with the electrical and chemical signals neurons use to communicate. Imagine trying to tune into your favorite radio station, but static drowns out the signal; eventually, the station fades away. That’s what happens when these proteins gum up the machinery of synaptic communication.
Over time, neurons struggle to form new synapses and maintain old ones. The presynaptic terminals the tiny boutons where messages are sent lose their natural rhythm of turnover. Instead of a dynamic system ready to adapt to new experiences, the network grows rigid, unable to encode fresh memories or update old ones. Scientists have observed this both in the brains of people with Alzheimer’s and in animal models engineered to mimic the disease.
This breakdown in communication explains why Alzheimer’s patients can often remember songs from their youth but not what they had for breakfast. The long-established circuits remain, while new ones can’t take shape. And as the disease advances, even older connections crumble.
What Brain Stimulation Actually Is And How It Works

At its core, brain stimulation is about nudging the brain’s circuitry back into rhythm. It doesn’t replace lost neurons or magically erase amyloid plaques. Instead, it delivers carefully tuned pulses of energy magnetic or electrical that encourage dormant connections to fire again, strengthening the pathways that memory depends on.
The most widely studied technique is repetitive transcranial magnetic stimulation (rTMS). A coil placed on the scalp generates brief magnetic pulses, which in turn create small electric currents in targeted brain regions. These currents can boost or calm neural activity depending on the frequency used. Think of it like tapping a rhythm on a piano string the right tempo can make the whole instrument resonate. rTMS is already FDA-approved for depression, which gives scientists confidence in its safety profile, and trials are now testing how it affects memory circuits disrupted in Alzheimer’s.
Another noninvasive method is transcranial direct current stimulation (tDCS). Instead of magnetic pulses, it uses a gentle electrical current passed between electrodes on the scalp. This current doesn’t force neurons to fire but makes them slightly more or less likely to do so, priming the brain to strengthen certain pathways. It’s less precise than rTMS but easier to administer and relatively low cost.
More invasive approaches aim deeper. Deep brain stimulation (DBS) requires surgically implanting electrodes into memory-related structures like the fornix or nucleus basalis. These electrodes are connected to a pulse generator placed under the skin of the chest, delivering continuous stimulation. DBS has shown intriguing benefits in early-stage Alzheimer’s but carries surgical risks such as infection or bleeding.
Finally, there’s vagus nerve stimulation (VNS), which influences brain function indirectly by sending signals through the vagus nerve a major communication highway between the body and brain. VNS can be invasive, with implanted devices, or noninvasive, using external stimulators placed on the skin near the neck or ear. Early results suggest mild cognitive improvements, but much more research is needed.
Each technique comes with its own trade-offs: rTMS and tDCS are noninvasive and safe but reach mainly surface-level networks, while DBS can access deep memory hubs at the cost of surgery. The common goal, however, is the same to restore a brain that has grown too quiet, by reawakening the conversations between its cells.
Animal Studies And Human Trials
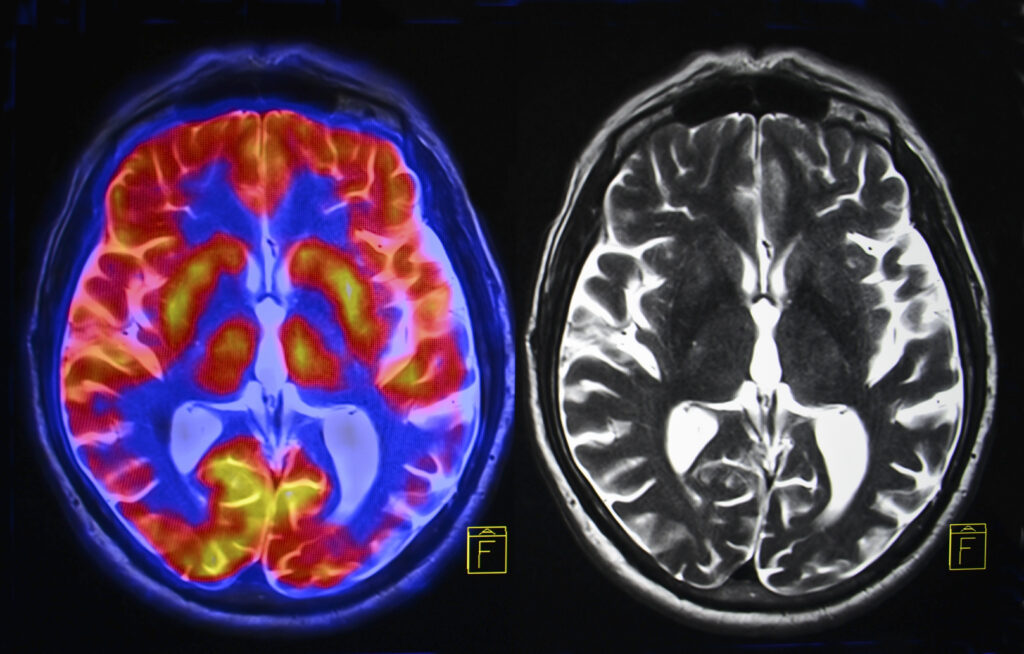
In animal studies, researchers at the University of Queensland and the University of Tasmania tested low-intensity repetitive transcranial magnetic stimulation (rTMS) on mice genetically engineered to develop Alzheimer-like pathology. Using two-photon microscopy, they tracked the synaptic boutons tiny swellings where neurons release signals. In healthy mice, these boutons are constantly turning over, a sign of flexibility. In the Alzheimer’s model, turnover slowed dramatically. But after just a single session of rTMS, the bouton turnover jumped by more than 200 percent, temporarily restoring it to levels seen in healthy animals. This wasn’t just noise in the data; it was a measurable shift in how neurons adapted and rewired, suggesting that stimulation can directly repair one of the disease’s most fundamental breakdowns.
Human trials, while still early, tell a complementary story. In a phase 2 trial presented in Madrid, 32 people with Alzheimer’s received weekly sessions of targeted rTMS for a year. Researchers zeroed in on the brain’s default mode network, a hub for autobiographical memory that is hit hard in the disease. Compared with participants who received sham treatments, those who underwent real stimulation experienced a 44 percent slower rate of cognitive decline. Even more importantly, they retained their ability to manage daily activities for longer an outcome that matters deeply to patients and families alike.
The numbers stack up surprisingly well against existing drugs. The newest antibody infusions, lecanemab and donanemab, slow decline by around 22 to 27 percent but carry risks of brain swelling and microbleeds, alongside annual costs exceeding $25,000. By contrast, the side effects of rTMS in the Alzheimer’s trial were mostly limited to mild headaches or scalp discomfort.
Other human studies add nuance. Small experiments with transcranial direct current stimulation (tDCS) have shown short-term gains in memory tasks. Deep brain stimulation (DBS) of the fornix has produced improvements in glucose metabolism and hippocampal volume in some patients, though results vary and the risks are greater. Vagus nerve stimulation (VNS) has shown hints of stabilizing cognition in tiny pilot trials, but the evidence is still thin.
How And Why Stimulation Might Help Memory
When researchers deliver magnetic or electrical pulses, they don’t force neurons to fire randomly. Instead, they shift the balance of excitability in targeted networks. In Alzheimer’s, this balance is off: excitatory signals like glutamate falter, inhibitory systems overcompensate, and the circuits lose their fine-tuned rhythm. Stimulation appears to reset that rhythm, nudging neurons into a state where they are more ready to form or strengthen connections.
There’s also evidence that stimulation boosts brain-derived neurotrophic factor (BDNF), a growth-supporting molecule often called “fertilizer for neurons.” Higher BDNF levels encourage synapse formation and help existing cells survive the toxic stress of amyloid and tau buildup. In animal studies, rTMS has restored bouton turnover the tiny synaptic release points bringing flexibility back into circuits that had grown rigid.
Beyond synaptic repair, stimulation may also reduce inflammation in the brain and help clear out some of the harmful protein clumps that clog communication. These effects are still being mapped out, but they suggest that stimulation doesn’t just make neurons more active it may also create a healthier environment for them to thrive.
What ties all this together is the idea that memory depends less on the sheer number of neurons and more on how flexibly they connect. By restoring plasticity, stimulation reopens the possibility for learning, remembering, and adapting. It’s not a cure, but it’s a way of reclaiming some of the brain’s natural resilience a spark of repair in circuits that had gone quiet.
Guidance for Patients and Caregivers

The first and most important point: these therapies are not cures. The strongest evidence so far comes from patients in the early or moderate stages of Alzheimer’s, where stimulation seems to slow decline or preserve daily function. That means the technology may be most useful as an added tool complementing medications, lifestyle changes, and supportive care rather than as a stand-alone solution.
For caregivers, this opens a handful of concrete actions. Asking a neurologist about ongoing clinical trials is one place to start. Many large hospitals and research centers are enrolling participants in studies of rTMS or related techniques. Participation not only offers access to emerging treatments but also provides close monitoring by specialists who understand the disease.
It’s also important to manage expectations. Even in the most promising trial, benefits were measured in slowed decline and preserved independence, not in dramatic restoration of memory. A patient may still forget new names or recent events, but they may retain more of their daily abilities for longer things like preparing a meal, recognizing loved ones, or following a conversation. Those small victories can make a meaningful difference for both patient and family.
Sessions themselves are typically straightforward. Noninvasive methods like rTMS involve sitting in a chair while a magnetic coil rests on the scalp. Treatments last around 20 minutes, often once or twice a week, with side effects limited to mild headache or scalp discomfort. For caregivers, this means the procedure can be folded into normal routines without the recovery time that comes with surgery or heavy medication.
In the meantime, proven strategies still matter. Regular exercise, good sleep, a balanced diet, mental challenges, and social connection all support brain health and may make stimulation therapies more effective when combined. Think of these habits as the soil in which any new treatment has to grow.
Restoring the Music of Memory
Alzheimer’s takes more than memory it steals connection. It unravels the threads that tie people to their own stories and to the people they love. Brain stimulation will not reverse the disease, and it will not restore a lifetime of memories in one dramatic flash. But what it can offer, even at this early stage, is something profoundly human: more time with the self intact, more moments where recognition holds, more space for dignity in the face of decline.
The science is still young, and caution is warranted. Larger trials, biomarker validation, and ethical guardrails are essential before these therapies become standard. Yet the promise is undeniable. Unlike treatments that only try to slow the buildup of harmful proteins, stimulation seeks to restore the brain’s ability to adapt and rewire to make the neural conversation possible again. That shift is not just medical; it is philosophical. It reframes Alzheimer’s not only as a story of inevitable loss but as one where resilience can be sparked, even in fading circuits.
For patients and caregivers, the path forward lies in a balance: hope without illusion, action without desperation. Stay informed, ask about clinical trials, support research, and nurture the everyday habits that keep the brain healthier for longer. Science is moving, and for once, it is moving toward a therapy that aims to rebuild rather than merely slow decay.
If Alzheimer’s is a disease of silence, brain stimulation is a chance however limited for the music of memory to play a little longer. And in that added time, there is meaning, there is presence, and there is hope.
Loading...

