Scientists Restored Hearing in People Born Deaf by Fixing This Faulty Gene With Viral Gene Therapy
What does silence sound like when it isn’t a choice? For millions of children born deaf, the world begins without the texture of a parent’s laugh, the rhythm of music, or the simple warning of a car approaching. Deafness has always carried with it more than just the absence of sound it has meant barriers to language, education, and connection.
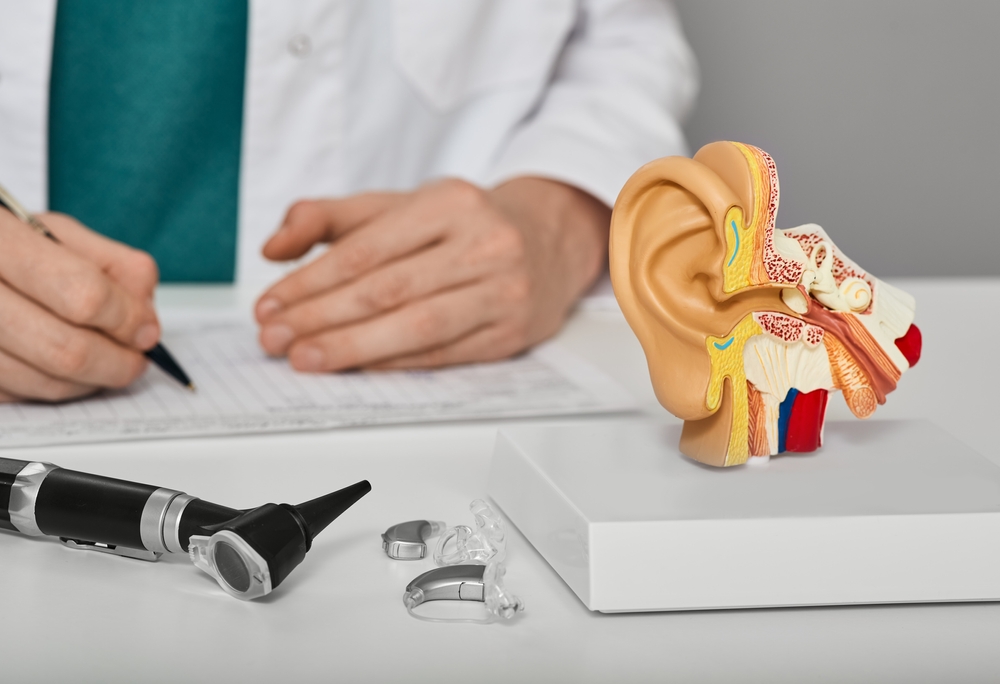
Globally, more than 1.5 billion people live with some form of hearing loss. For decades, the best science could offer were devices: hearing aids to amplify muffled sounds, or cochlear implants that bypass damaged pathways and deliver electrical signals straight to the brain. These tools have changed lives, but they cannot recreate the delicate symphony of natural hearing. For children with certain genetic forms of deafness, even these options bring limited hope.
That’s why what scientists have recently achieved is nothing short of astonishing. By fixing a single faulty gene with viral gene therapy, they have given children born deaf the ability to hear for the first time. Some heard sound within days. Others, after months of silence, began to recognize words and music.
It is more than a medical milestone it is proof that silence, once thought permanent, can be broken.

The Silent Weight of Hearing Loss
Hearing loss isn’t just about missing sounds it’s about missing pieces of life. Conversations become exhausting puzzles, classrooms turn into barriers instead of gateways, and social gatherings transform into isolating spaces. The ripple effects go deeper than many realize. Studies link untreated hearing loss not only to social isolation and depression but also to cognitive decline and dementia in later life.
The scale of the issue is staggering. More than 1.5 billion people worldwide live with some form of hearing loss, according to the World Health Organization. About 30 million children are affected by genetic forms of impairment, and up to three in every 1,000 newborns are born with hearing loss in one or both ears. For those children, the silence starts from day one and unless something changes, it lasts a lifetime.
The most common cause of permanent hearing loss is sensorineural hearing loss (SNHL). Unlike conductive hearing loss, which blocks sound before it reaches the inner ear, SNHL begins inside the cochlea, the spiral-shaped organ deep within the skull. Here, specialized hair cells and neurons translate sound waves into electrical signals and pass them to the brain. When these fragile cells are damaged for when the neurons that carry their messages break down the chain of communication is lost. The brain is ready to listen, but the ear can no longer deliver the message.
Hearing restored in rats by modifying ear cells to respond to light https://t.co/rQ9GzTq29F pic.twitter.com/XC4p9Cujq5
— New Scientist (@newscientist) July 22, 2020
Modern medicine has done what it can. Hearing aids amplify sound for those with mild to moderate loss. Cochlear implants bypass the damaged cells entirely, sending electrical signals directly to the auditory nerve. These devices are nothing short of revolutionary, but they are not perfect. Hearing aids cannot restore what is gone, only boost what remains. Cochlear implants, while life-changing, require invasive surgery and still can’t capture the full nuance of natural hearing the layered harmony of music, the subtle inflection in a loved one’s voice.
What makes this even more devastating is that humans are born with all the hearing cells they will ever have. Once these cells die, they don’t regenerate. In other words, for much of history, hearing loss has been a one-way street: once the cells are gone, silence is forever.
The Science of Hearing and the OTOF Gene
To understand why this breakthrough matters, we need to step inside the inner ear, a marvel of biological engineering packed into a chamber no larger than a pea. At the heart of this system sits the cochlea, a spiral-shaped organ filled with fluid and lined with thousands of sensory hair cells. These hair cells don’t resemble the hair on your head; instead, they look like tiny bristles that sway when sound vibrations ripple through the cochlea.
Each sway sets off an electrical signal. But the hair cells can’t communicate with the brain on their own. They rely on a molecular middleman: a protein called otoferlin, produced by the OTOF gene. Otoferlin acts like a translator, packaging the sound information into signals that auditory neurons can carry up the auditory nerve to the brain. This is how vibrations transform into something as rich as a symphony or as intimate as a whispered “I love you.”
When the OTOF gene is faulty, otoferlin is either missing or broken. The hair cells may be perfectly healthy and capable of detecting sound waves, but without otoferlin, the message stalls. It’s like having a microphone that can pick up sound but no wire to carry the signal to the speaker. The result is profound deafness from birth, even though the inner ear structures remain intact.
This is what makes OTOF-related deafness such an ideal target for gene therapy. Unlike other forms of hearing loss, where cells have been destroyed and must be rebuilt, here the “machinery” is still in place. The only missing piece is the functioning gene. In theory, if you replace or repair that single faulty instruction manual, the system should come back online.
Globally, around 200,000 people live with this rare form of congenital deafness. While the number may seem small compared to the vast population living with hearing loss, OTOF offers something bigger than just a treatment for one condition. It represents a test case for whether gene therapy can do what medicine has never done before: restore natural hearing by addressing the root cause.
The Breakthrough Trials Restoring Hearing with Gene Therapy

The research teams in China, the United States, and the United Kingdom recruited children and young adults, ranging from toddlers to 24 years old, all born with OTOF-related deafness. Each participant received a single injection of the viral vector directly into the cochlea. The virus acted as a courier, attaching itself to the surface of the inner ear’s hair cells and slipping inside. Once there, it released the working gene, giving the cells the missing instructions to produce otoferlin.
One major hurdle was the size of the OTOF gene itself it was too large to fit into the viral “container” typically used for gene therapy. Researchers overcame this by splitting the gene into two parts, packaging each half into separate viral vectors, and injecting them together. Inside the cell, the halves reassembled, and for the first time, the broken communication system between hair cells and neurons was restored.
The results were astonishing. In clinical trials, patients showed rapid and measurable improvements. Objective brainstem response tests revealed an average 62% improvement in the first month. Behavioral hearing assessments where participants pressed a button or raised a hand when they detected a faint beep showed a 78% improvement. For some, progress was almost immediate. A seven-year-old girl reportedly reacted to sound just three days after treatment, startling both her parents and the medical team.
By the end of the 12-month study period, children who had lived in silence were recognizing speech, responding to voices, and even beginning to develop spoken language. In five of six children treated in one trial, the ability to perceive speech improved dramatically, with some able to hold conversations in noisy rooms or over the phone. One mother recalled the life-changing moment when her daughter turned her head at the sound of her voice something she had never done before.
Equally important, the treatment proved safe. Across trials involving multiple hospitals, participants experienced only mild side effects, such as temporary drops in white blood cell counts. No serious adverse events were reported, offering reassurance that this revolutionary therapy could be both effective and safe for children.
“This really opens the door to developing other treatments for different kinds of genetic deafness,” said Dr. Zheng-Yi Chen of Harvard Medical School, one of the trial leaders. His colleague, Dr. Yilai Shu at Fudan University, described the moment parents realized their children could hear as “emotional beyond words.” Many wept as silence gave way to sound.
The Future of Hearing Restoration
As extraordinary as these results are, OTOF-related deafness is rare, affecting an estimated 200,000 people worldwide. Most hearing loss isn’t caused by a single faulty gene but by a lifetime of wear and tear, noise exposure, illness, or aging. That reality raises the question: what about the millions whose hearing loss cannot be traced back to one broken instruction in their DNA?
This is where regenerative medicine steps in. Researchers at the University of Sheffield and the biotech company Rinri Therapeutics are developing cell-based therapies that could address the far more common forms of sensorineural hearing loss. Instead of fixing a gene, their approach involves creating new auditory nerve cells from stem cells and implanting them directly into the cochlea. These cells can potentially replace those lost to age, trauma, or disease something no device or drug has ever been able to do.
The early results in animals have been nothing short of promising. In preclinical models, implanted cochlear neurons derived from stem cells produced a dramatic ~25 decibel improvement in hearing thresholds. If replicated in humans, that difference could mean going from being unable to hear traffic on a street to being able to carry on a conversation in a room. Rinri’s therapy, known as Rincell-1, is now preparing for the first human trials in 2025 a potential medical milestone.
But the challenges remain formidable. The cochlea is buried deep inside one of the hardest bones in the human body, making it notoriously difficult to access. Delivering delicate cells or genes with precision requires surgical skill at the highest level. To overcome this, researchers are pioneering new imaging techniques and surgical pathways, refining how therapies can be delivered safely to this hidden organ.
Meanwhile, scientists are also pushing gene therapy beyond OTOF. Other, more common forms of genetic deafness involve multiple mutations or more complex pathways. While harder to solve, progress in animal studies suggests it may be possible to develop tailored therapies for these conditions as well. The OTOF breakthrough offers a crucial proof of concept: once you can restore hearing by fixing one gene, the door is open to tackling many more.
The Broader Implications Medicine’s Genetic Frontier

The restoration of hearing through gene therapy is more than a victory over one form of deafness it’s a glimpse into the next chapter of medicine. For centuries, doctors have treated symptoms. In recent decades, we’ve learned how to manage disease with drugs, implants, and devices. But with gene therapy, medicine is entering a new era: one where we correct the root cause, rewriting the body’s code so that illness itself is undone.
This shift is already being felt across multiple fields. In 2023, the U.S. approved the first gene-editing treatment for sickle cell disease, offering a one-time therapy for a condition that has plagued families for generations. Experimental gene therapies have restored partial vision to patients with certain types of inherited blindness. In neurology, scientists are exploring treatments for muscular dystrophy and Parkinson’s disease that use the same principles now restoring hearing in deaf children.
But these scientific triumphs also raise profound questions. Who will have access to such treatments, and at what cost? Cutting-edge therapies often carry price tags in the hundreds of thousands of dollars, creating a chasm between what’s scientifically possible and what’s socially equitable. Will breakthroughs be reserved for the wealthy few, or will they eventually become part of standard care, accessible to all?
There are also questions about durability. Will the restored hearing last a lifetime, or will patients need booster treatments? How will regulators ensure safety as more experimental therapies move rapidly from labs into clinics? These aren’t reasons to slow progress, but they are reminders that science doesn’t exist in a vacuum it unfolds in human lives, shaped by policy, ethics, and economics.
Still, the broader implication is undeniable: we are standing at the edge of a paradigm shift. The ability to fix a faulty gene and restore hearing in children born deaf is a proof of concept that stretches far beyond the ear. It shows that the body’s code is not destiny that silence, blindness, or genetic disease may no longer be permanent sentences. The same tools used to give a child their first experience of sound may one day rewrite the future of medicine itself.
A World Where Silence Can Be Broken
For most of human history, deafness at birth meant a lifetime of silence. Families adapted, communities supported, technology offered partial answers but the underlying silence remained. Now, with the success of gene therapy in restoring hearing, that silence has been cracked open. Children who once knew only stillness are beginning to hear voices, laughter, and music for the first time.
This is not just a story about ears or genes. It is about possibility. It shows us what happens when science dares to move past limitation and into imagination when researchers refuse to accept that something is irreversible. The work being done on the OTOF gene, and the cell therapies waiting in the wings, are symbols of a broader truth: the boundaries of what we call “incurable” are shifting.
There are challenges ahead making these therapies affordable, ensuring long-term safety, expanding them to more common forms of hearing loss. Yet even with those hurdles, one fact remains: the silence has been broken. And in that sound, there is a promise not only for those who live with deafness, but for all of us who wonder what else science might one day restore.
The day is coming when hearing loss may not be managed, but cured. And when that happens, the first sound many will hear won’t just be a voice or a note of music it will be the echo of human determination saying, again and again, nothing is truly impossible.
Loading...

