Scientists Discover New Blood Type Only Found in One Woman on Earth Today
Something happened in a Paris laboratory that would make one woman the most medically unique person on Earth. Scientists discovered that her blood contained something they’d never seen before – something so rare that after decades of searching, she remains the only known person to possess it.
Imagine going for routine medical tests and learning that your blood is incompatible with every other person on the planet. Picture being told that if you ever needed a blood transfusion, the only person who could save your life is yourself. This isn’t science fiction – it’s the reality for one remarkable woman whose genetic makeup defies every established rule about human blood compatibility.
What started as a simple pre-surgery blood test in 2011 became a medical mystery that would take scientists eight years to solve. When they finally cracked the code, they realized they had discovered something that would rewrite textbooks and challenge everything doctors thought they knew about human blood.
But how does someone end up being the only person on Earth with their blood type? What does this mean for her survival? And are there others like her hidden somewhere in the world, waiting to be discovered?
Meet the Woman Who Is Only Compatible with Herself
At 68 years old, a woman from the Caribbean island of Guadeloupe holds a distinction that no other human being shares. French scientists have confirmed that she possesses a blood type found nowhere else on Earth – a genetic combination so unique that medical experts describe her situation in terms that sound almost surreal.
“She is the only person in the world who is compatible with herself,” explained Thierry Peyrard, a medical biologist involved in the groundbreaking discovery. This statement carries profound implications that extend far beyond simple medical curiosity.
Living with this knowledge means accepting that traditional emergency medicine safety nets don’t apply to her situation. While most people can receive O-negative blood in emergencies – the so-called universal donor type – this woman faces a completely different reality. Her immune system would attack any foreign blood as a dangerous invader, potentially causing fatal reactions.
Scientists have named her blood type “Gwada negative,” honoring her Caribbean heritage with a phonetic reference to Guadeloupe that sounds pleasant in multiple languages. But behind this friendly designation lies a sobering medical truth: she represents a population of one.
2011 Mystery: A Routine Blood Tests Revealed the Impossible

The discovery began with what should have been a straightforward medical procedure. In 2011, when the woman was 54 years old and living in Paris, she underwent routine blood tests before scheduled surgery. Laboratory technicians immediately noticed something unusual in her samples.
Her blood contained antibodies they had never encountered before. Standard blood typing procedures failed to categorize her samples properly. Something in her genetic makeup was producing immune responses that didn’t match any known blood group system.
Scientists recognized they were observing something significant, but technology limitations prevented them from investigating further. The case went cold, filed away with other medical mysteries waiting for scientific advances to provide answers.
For eight years, this woman continued her life unaware that her blood held secrets that would eventually reshape medical understanding of human genetic diversity. Her routine surgery proceeded successfully, but the mystery of her unique blood type remained unsolved.
DNA Detectives Crack the Case in 2019
Advanced genetic analysis technology finally caught up with the mystery in 2019. High-throughput DNA sequencing capabilities had improved dramatically, allowing scientists to examine genetic material with unprecedented detail and speed.
Researchers decided to revisit the puzzling 2011 case, applying new analytical techniques to stored blood samples. Two years of intensive research followed, during which scientists sequenced the woman’s entire genome looking for explanations.
The breakthrough came when they identified a mutation in a gene called PIGZ. This genetic alteration affects how proteins attach to the surface of red blood cells, fundamentally changing their chemical signature and immune system recognition patterns.
Gene sequencing revealed that both of the woman’s parents had carried the mutated PIGZ gene. When she inherited altered copies from both parents, the combination created something completely new in human blood typing – a genetic lottery that produced a one-person blood group.
Welcome to Blood Group 48: “Gwada Negative” Joins the Club

The International Society of Blood Transfusion officially recognized this discovery in June 2025, designating “Gwada negative” as the 48th known blood group system. This recognition represents the culmination of decades of research and places the discovery among the most significant advances in transfusion medicine.
“The EFS has just discovered the 48th blood group system in the world!” announced the French Blood Establishment, which has been responsible for identifying 10 of the last 17 blood groups discovered globally.
Blood group systems represent far more complexity than most people realize. While everyone learns about A, B, AB, and O types in school, medical professionals work with dozens of additional classification systems based on various antigens and antibodies present in human blood.
Each new discovery helps doctors provide safer transfusions and better understand human genetic diversity. But Gwada negative presents unique challenges because it exists in only one known person, making compatibility research particularly difficult.
How Two Parents Created Medical History
Understanding how someone develops such a rare blood type requires examining the genetic inheritance patterns that created this unprecedented situation. Blood types result from specific gene combinations passed down from parents to children.
In this case, both parents carried mutations in their PIGZ genes but likely had normal blood types themselves because they possessed one normal copy alongside the mutated version. When their daughter inherited mutated copies from both parents, the combination produced effects that neither parent experienced individually.
PIGZ gene mutations alter how proteins anchor to red blood cell surfaces. These protein attachments serve as identification markers that help the immune system distinguish between “self” and “foreign” substances entering the bloodstream.
When both copies of the PIGZ gene carry specific mutations, the resulting protein patterns create blood cell signatures that no other human immune system recognizes as familiar. This genetic combination appears to be extraordinarily rare, possibly occurring only once in recorded medical history.
When Universal Donors Don’t Work

Most people take for granted that O-negative blood provides a safety net during medical emergencies. Hospitals stock O-negative blood specifically because it rarely causes adverse reactions in recipients, earning its designation as the universal donor type.
For the woman with Gwada negative blood, this universal compatibility doesn’t exist. Her immune system would recognize even O-negative blood as foreign material and mount aggressive attacks against transfused cells. Such reactions can cause kidney failure, circulatory collapse, and death within minutes.
This incompatibility extends beyond red blood cells to include plasma and platelet transfusions. Traditional blood banking approaches simply don’t work for someone whose immune system has never encountered compatible donor material from other humans.
Medical emergencies become exponentially more dangerous when standard treatment protocols could prove fatal. Every surgical procedure, accident, or health crisis requires special preparation and alternative treatment strategies.
Building Your Own Blood Bank
Faced with complete incompatibility with all other human blood, this woman must serve as her own donor. Medical teams have established protocols for regular blood donations that create emergency reserves specifically for her future needs.
Autologous blood donation – giving blood for your own future use – typically involves drawing blood several weeks before planned surgeries. For someone with Gwada negative blood, this becomes a lifelong necessity rather than an occasional precaution.
Stored blood has limited shelf life, requiring careful rotation and replacement to maintain fresh supplies. Red blood cells can be preserved for about 42 days under optimal conditions, while frozen blood products last longer but require special handling and preparation.
Creating adequate blood reserves for emergency situations requires ongoing medical supervision and storage facilities capable of maintaining proper temperatures and sterile conditions. This woman’s survival depends on infrastructure that most people never need to consider.
Scientific Treasure Hunt: Searching for Others Like Her

Despite her apparent uniqueness, scientists haven’t given up hope of finding other people with Gwada negative blood. Genetic traits often cluster within populations sharing common ancestry, suggesting that relatives or people from similar backgrounds might carry the same mutations.
Research teams are focusing their search on Guadeloupe, where genetic testing of blood donors might reveal additional cases. Family members represent the most likely candidates for sharing similar blood type characteristics, even if they don’t possess identical mutations.
Population genetics research indicates that rare genetic traits sometimes persist in isolated communities for generations. Caribbean populations might harbor other individuals with PIGZ gene mutations that haven’t been medically documented yet.
Finding even one additional person with compatible blood would transform this woman’s medical situation from impossible to merely complicated. Two people with the same rare blood type could potentially serve as donors for each other during emergencies.
Why This Discovery Matters So Much
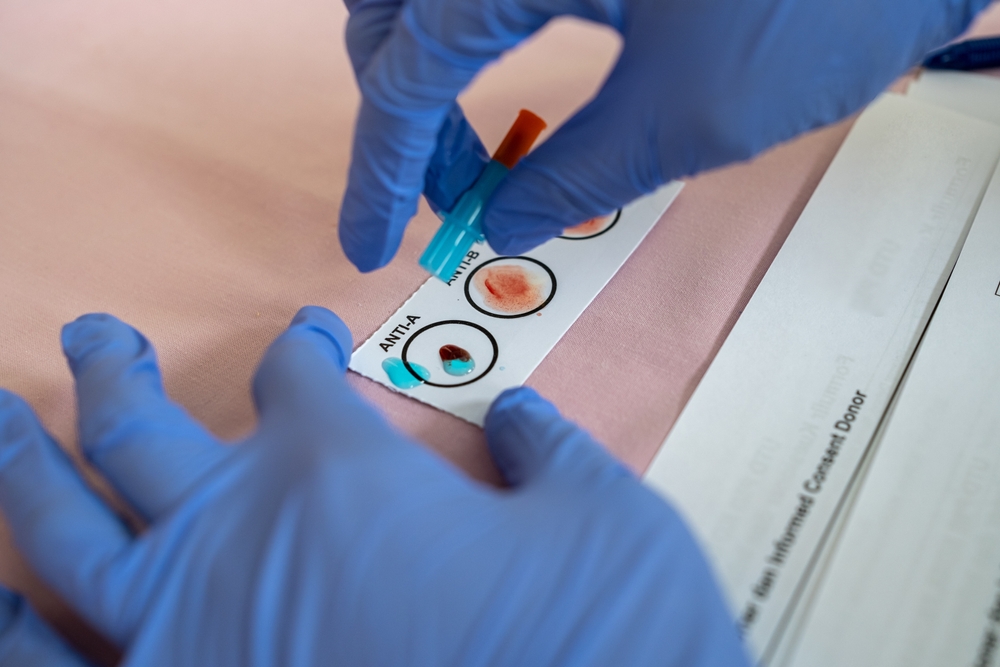
Blood compatibility depends on complex interactions between antigens present on red blood cell surfaces and antibodies circulating in blood plasma. When incompatible blood mixes, antibodies attack foreign antigens, causing cells to clump together and block circulation.
The ABO system discovered in 1901 established the foundation for safe blood transfusions by identifying four basic blood types based on A and B antigens. Rh factor classification added positive and negative designations, creating eight commonly recognized blood groups.
However, scientists have since discovered dozens of additional blood group systems based on other antigens and genetic variations. Each system represents different ways that human immune systems distinguish between self and foreign blood components.
Gwada negative blood contains antigen patterns that don’t match any previously known system. The woman’s immune system produces antibodies against essentially all other human blood types, making her medically isolated from potential donors worldwide.
Living as a Medical Unicorn
Being the world’s only known person with your blood type creates psychological pressures that extend far beyond medical concerns. Every day involves awareness that standard emergency care protocols don’t apply to your situation.
Travel requires careful planning and communication with medical facilities about special blood storage needs. Medical identification jewelry and cards must clearly communicate the impossibility of using standard blood products during emergencies.
Building relationships with specialized medical teams becomes essential for managing routine healthcare needs. Few doctors encounter patients requiring such unprecedented blood compatibility considerations during their careers.
The woman has adapted to her unique situation with remarkable resilience, but the constant awareness of medical vulnerability affects decisions about activities, travel, and lifestyle choices that most people take for granted.
From Hidden Twins to Lab-Grown Blood
Research continues as scientists search for other individuals who might share similar genetic mutations. International collaboration between blood banks and genetics laboratories increases the chances of identifying additional cases.
Development of artificial blood substitutes might eventually provide alternatives for people with extremely rare blood types. Laboratory-grown blood products could offer compatibility solutions when human donors aren’t available.
Gene therapy approaches might someday allow modification of blood cell characteristics to improve compatibility options. While such treatments remain experimental, they represent potential future solutions for genetic blood disorders.
The story of Gwada negative blood reminds us that human genetic diversity continues surprising scientists and challenging medical assumptions. In a world of eight billion people, one woman stands alone with blood that makes her truly one of a kind.
Loading...

