Creating a Kidney for Everyone the Next Evolution in Medicine

The idea of a universal donor kidney sounds like something out of a futuristic medical drama: a single organ capable of saving anyone, regardless of blood type. Yet this concept is no longer the stuff of science fiction. In recent years, researchers in the United Kingdom, the United States, and China have demonstrated the ability to alter the blood type of human kidneys, transforming them into universal donor organs. These scientific milestones may soon revolutionize transplant medicine, potentially ending one of the most stubborn inequities in healthcare. But beyond the headlines about life-saving breakthroughs lies another layer of inquiry: how much could this cost, who will benefit first, and what does it mean for the future of medicine?
The Problem of Compatibility
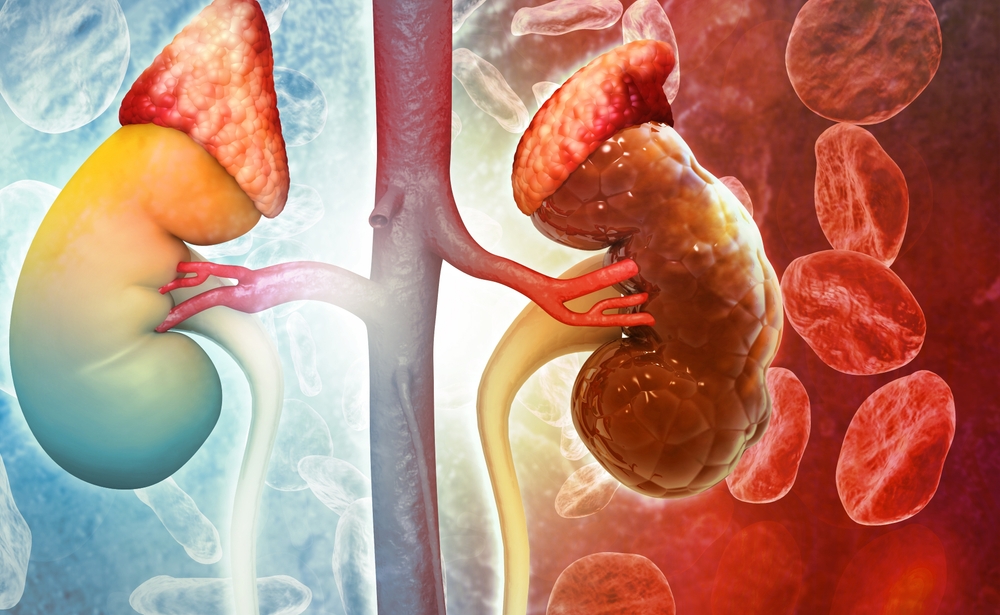
For decades, one of the greatest obstacles in organ transplantation has been blood type compatibility. Human blood types are determined by antigens, which are small molecules on the surface of red blood cells and blood vessels. These antigens A, B, AB, or O dictate whether the body will accept or reject foreign tissue. If someone with type A blood receives a type B kidney, their immune system will recognize the antigens as invaders and destroy the organ. This immune reaction, called rejection, can occur within minutes and is almost always fatal to the transplanted tissue.
For kidney transplants, this means matching donors and recipients by blood type is essential. Unfortunately, this requirement also means many patients wait years for a compatible organ. In the United States alone, over 90,000 people are currently on the waiting list for a kidney transplant. Roughly half of them have type O blood, which is the most universal donor type but the most difficult to match. Type O recipients can only receive kidneys from other type O donors, creating a long bottleneck in an already overstressed system.
The situation is even more severe in minority ethnic communities. In the UK, for instance, Black and South Asian patients wait, on average, a year longer for a kidney than white patients. That gap exists because blood types and tissue markers are influenced by genetic ancestry. Minority patients are more likely to have rarer blood types such as B, yet organ donation rates among those groups remain disproportionately low. The result is a tragic imbalance where patients from these communities often die waiting for transplants that could have saved their lives.
The Science Behind the Breakthrough
At the University of Cambridge, a team led by transplant surgeon Professor Mike Nicholson and PhD researcher Serena MacMillan has been developing a way to sidestep blood type incompatibility altogether. Using a technology called a normothermic perfusion machine, they can pump oxygenated blood and enzymes through a kidney outside the body, effectively keeping it alive while modifying it. The key lies in special enzymes that act like molecular scissors, removing the A or B antigens from the blood vessels of the kidney.
When the Cambridge team treated B-type kidneys with these enzymes, the organs were converted to type O in just a few hours. The transformation was confirmed when the once B-type kidneys no longer triggered immune reactions to A or B blood. In essence, they had created universal donor kidneys that could, in theory, be transplanted into anyone.
Researchers in China and North America have since taken the idea further. In one recent experiment published in Nature Biomedical Engineering, scientists successfully transplanted a converted type A kidney into a brain-dead patient. For two days, the kidney functioned normally, filtering waste and producing urine without signs of rejection. On the third day, however, the A antigens began to reappear, prompting an immune reaction. While temporary, the result proved that the concept works in a real biological system. The next challenge will be finding ways to make the antigen removal permanent.
The discovery of this enzyme-based method has roots in earlier research on blood transfusion compatibility. In 2019, scientists at the University of British Columbia identified two enzymes derived from gut bacteria that could strip A and B antigens from red blood cells. The Cambridge and Chongqing teams later adapted those enzymes for use in solid organs. By perfusing the kidney with an enzyme-rich solution, they could erase its antigenic identity, leaving a blank slate recognizable by any blood type.
From Experiment to Clinical Reality

As promising as this technology sounds, the journey from laboratory success to clinical routine is long and costly. Before universal donor kidneys can be used in living patients, researchers must confirm that the conversion process does not damage the organ or lead to unexpected immune complications. They also need to understand how long the antigen-free state lasts and whether it might trigger new, subtler forms of rejection once transplanted.
At present, testing is limited to ex vivo studies and trials in brain-dead donors with family consent. These controlled experiments help scientists measure how the converted kidneys interact with different blood types under realistic conditions. Once these tests confirm safety, the next stage will involve small-scale clinical trials in living patients who consent to receive an enzyme-converted organ. Regulators such as the UK’s Medicines and Healthcare Products Regulatory Agency and the US Food and Drug Administration will then need to approve wider trials before any hospital can offer such transplants routinely.
That process could take five to ten years and cost tens of millions of dollars. Beyond the scientific hurdles, there are logistical and ethical questions to resolve. Will enzyme conversion be performed on every donor kidney as a standard step, or reserved only for mismatched cases? How will hospitals and insurers price such procedures, and will patients from lower-income backgrounds have access? These questions will shape how the technology evolves and whether it fulfills its humanitarian promise or becomes another medical privilege.
The Cost of Creating a Universal Organ

Estimating the cost of a universal kidney is tricky because the technology is still experimental. However, we can make educated guesses by looking at the components involved. A normothermic perfusion machine costs between $50,000 and $150,000, depending on the model and capabilities. Each enzyme treatment would add another few thousand dollars per organ. Factoring in research, staffing, and maintenance, early-stage enzyme-converted kidney procedures could easily exceed $200,000 per transplant.
For comparison, a standard kidney transplant in the United States typically costs around $400,000, including surgery, hospitalization, and post-operative care. Much of that cost comes from lifelong immunosuppressive drugs, which can run tens of thousands of dollars per year. If enzyme-converted kidneys reduce the need for intense immune suppression or shorten waiting times, they might eventually lower total healthcare costs in the long run. But in the near future, they will likely be more expensive due to the specialized equipment and expertise required.
Economic models of new medical technologies often follow a predictable curve: high initial cost, rapid innovation, then price stabilization as the method becomes standardized. If the enzyme perfusion process proves reliable, it could become an add-on service performed in regional transplant centers. Over time, automation and economies of scale might bring costs down to a few thousand dollars per organ. In the same way that genetic sequencing dropped from billions of dollars to less than a hundred in two decades, universal organ conversion could become routine once the infrastructure matures.
The more profound question may not be the financial cost but the moral one. How much is society willing to pay for universal access to transplants? Every year, thousands of people die waiting for compatible kidneys. If a relatively modest investment could save those lives, the ethical calculus may favor swift adoption. Yet, as history shows, medical revolutions often widen inequalities before they narrow them. Wealthier hospitals and nations will likely gain access first, while poorer regions struggle to catch up. Bridging that gap will require deliberate global cooperation and policy planning.
The Spiritual Symbolism of Universality

Beneath the technical details of enzymes and blood markers lies a deeper symbolism that touches on the nature of life itself. The idea of a universal organ that can belong to anyone challenges traditional notions of identity and separation. Blood, after all, has always been a symbol of individuality and connection. It carries our genetic heritage and our sense of self, yet it also unites us in the shared rhythm of life.
In many spiritual traditions, blood represents the essence of life that transcends individuality. Ancient texts describe it as the sacred carrier of spirit or soul. The fact that modern science can now modify blood identity at the molecular level evokes philosophical questions about what makes something part of “us.” When a kidney from one person can be reconfigured to suit another, we are reminded that our biological differences are not as fixed as they appear. Our bodies, like our societies, are built on systems of exchange and transformation.
From a metaphysical standpoint, the universal kidney reflects an evolution in human consciousness toward inclusivity. It is a material manifestation of a spiritual principle: that life seeks unity through diversity. Just as the body rejects what it perceives as foreign, societies often resist what they do not understand. In learning to harmonize with difference at the cellular level, we may also be learning something about compassion and cooperation on a larger scale.
Toward Universal Organs

The enzyme-based transformation of kidneys is only the beginning. Researchers have already tested similar methods on lungs, and there are plans to explore hearts and livers next. Theoretically, any organ that expresses A or B antigens could be converted to type O using the same process. This could lead to an entirely new paradigm in transplantation, where donor organs are routinely treated and stored in universal form, ready for any compatible recipient.
Parallel fields such as xenotransplantation the use of animal organs in humans may also benefit. Pig organs, for instance, could be genetically engineered to remove antigenic markers that trigger rejection, combining gene editing with enzyme treatment for optimal compatibility. The convergence of these technologies could one day make organ shortages a relic of the past.
Still, the scientific community remains cautious. Even if enzyme-converted kidneys prove safe, the long-term immune effects must be studied for decades. The immune system is extraordinarily complex, and subtle mismatches could cause chronic rejection years after transplantation. Researchers must also ensure that removing antigens does not make organs more vulnerable to infection or cancer.
The Future of Healing
Medicine has always advanced by redefining what is possible. Just as antibiotics once turned deadly infections into treatable conditions, the universal kidney could redefine our relationship with organ failure. But it also invites reflection on the boundaries between healing, identity, and ethics. When an organ can be made to fit any body, the distinction between self and other grows thinner. What once separated donor and recipient becomes a point of connection, a shared field of biological and spiritual unity.
As for the cost, it may be high at first, both financially and philosophically. But like all transformative technologies, its value will not only be measured in dollars saved or years gained. It will also be measured in the hope restored to those who have waited too long for a chance at life. In that sense, the universal kidney represents something more than a medical milestone. It is a reminder that the pursuit of science is, at its core, an act of compassion a way of extending life by transcending the boundaries that once defined it.
Loading...

